|
Skin problems
|
Introduction
Domestic animals are often afflicted with various skin problems, some easy to cure others more complicated, and some even highly contagious to the human handlers. The effect of skin problems on animal productivity also varies from mild irritations to rapid death, with all kinds of in between stages affecting the productivity and comfort of the animals. It really pays to pay close attention to the health and comfort of domestic animals.
Bovine Farcy
Scientific name: Bovine nocardiosis
Local names: Rendille: Ilmongoi, Somali: ghendiburr, Turkana: Etune, Pokot: rokon potich, Gabbra: Chawe, Maasai: erririe, entoki-keri
Description: Fungal disease
Introduction
This is a bacterial disease caused by Nocardia farcinica organisms. These organisms cause chronic, non-contagious diseases in animals and humans. They are commonly found in soil, decaying vegetation, compost and other environmental sources. They enter the body through contamination of wounds or by inhalation.
The disease in cattle is characterised by infection and swelling of the superficial lymphatic vessels and lymph nodes of the legs, neck and around the base of the ears.
Only cattle and humans are affected
Mode of spread
Transmission is by direct contact with affected animals, or indirectly via contaminated bedding, harnesses etc, or via infection of skin wounds.
Ticks may be involved in transmission. The prevalence of affected animals within a herd is usually low, but, on occasion, for reasons unknown, it may slowly spread until almost the whole herd is affected. The disease is more common in the drier, hotter, semi-arid areas of the country, where minor damage from skin wounds from thorny vegetation can occur and transmission by Amblyomma ticks is possible.
Signs of Bovine Farcy
The disease affects cattle of all ages.
It appears initially as small nodules under the skin, most often on the legs and on the neck, at the base of or near the ears. The nodules develop slowly, and some are grouped together in the form of a large mulberry. They are firm and painless. Infection slowly extends along the lymphatic vessels, which become prominent and corded, and along them more nodules may arise, together with the enlargement of the regional lymph nodes. Neither the nodules nor the lymph nodes show any tendency to rupture despite the latter sometime attaining the size of a large coconut. Swellings may persist for years with no apparent adverse effect on the health of the animal.
It appears initially as small nodules under the skin, most often on the legs and on the neck, at the base of or near the ears. The nodules develop slowly, and some are grouped together in the form of a large mulberry. They are firm and painless. Infection slowly extends along the lymphatic vessels, which become prominent and corded, and along them more nodules may arise, together with the enlargement of the regional lymph nodes. Neither the nodules nor the lymph nodes show any tendency to rupture despite the latter sometime attaining the size of a large coconut. Swellings may persist for years with no apparent adverse effect on the health of the animal.
On incision the swelling yields a thick, yellowish or greyish-yellow pus, sometimes granular in appearance and to the touch, but usually smooth and cheese-like. The abscesses show no tendency to resolve and ultimately spread to the internal organs leading to loss of condition and death.
Sometimes there is gross swelling of a leg when deeper tissues are involved. This is usually a more rapid, advancing form of the disease.
Diagnosis
This should present little difficulty. The cutaneous nodules, swollen lymphatic vessels, enlarged superficial lymph nodes, with little effect on the health of the animal, or in more severe cases, the enlarged limb together with the corded lymphatic vessels and swollen lymph nodes and loss of condition should leave little doubt as to the cause.
The lesions are essentially cheese-like abscesses, surrounded by a well-marked capsule of fibrous tissue. The lymphatic vessels are corded and thickened. Lesions of varying size may be found in internal organs, especially the lung and associated lymph nodes.
A veterinarian will confirm the diagnosis by smears of pus removed from an unopened abscess. The main concern is to distinguish the lesions of Bovine Farcy from those of Tuberculosis, which on occasion it can resemble, especially when there are internal lesions, such as those occurring within the chest cavity.
Treatment
There is no effective treatment
Cutting of the abscesses and the release of pus is of no value. Antibiotics likewise have no effect on the course of the disease.
Cutting of the abscesses and the release of pus is of no value. Antibiotics likewise have no effect on the course of the disease.
Prevention and Control
- Sporadic cases should be isolated and more severe cases slaughtered.
- Attention should be paid to tick and fly control, by regular spraying or dipping, with especial attention being paid to Amblyomma species of tick.
- Cattle should be moved out of thick, thorny vegetation, which can cause minor skin wounds and allow entry of infection.
- All minor skin wounds, from whatever cause, must be treated promptly and effectively.
- In some cases a slaughter/disposal policy may have to be implemented to effect control. A delay in implementing this may lead to a slow and inexorable spread throughout the herd.
Elephant Skin Disease (Besnoitiosis)
Elephant Skin Disease, or Besnoitiosis, is a disease of the skin, subcutaneous tissue, blood vessels, mucous membranes and other tissues caused by a protozoal parasite. It affects cattle, horses and donkeys and several species of wildlife. Goats occasionally get the disease. The affected animals are intermediate hosts. The final host of the organism responsible for disease in cattle is the cat. That of the horse is presently unknown. The disease occurs worldwide.
Mode of spread
Besnoitia besnoiti is the parasite responsible for the disease in cattle and various African wild ruminants and Besnoitia bennetti is responsible in horses and donkeys. The final hosts excrete Besnoitia oocysts in their faeces, which are then ingested in contaminated feed or water by the intermediate host. For the cycle to be completed in the case of cattle, a cat has to eat cysts that have been formed in the tissues of an infected cow.
The disease may also be spread mechanically by biting flies, such as tsetse flies, or by needle transmission.
Signs of Elephant skin disease
Bovine besnoitiosis occurs in cattle over six months old. The disease occurs in two stages.
Stage 1:
- About a week after infection, affected animals may have a high fever up to 41.67 °C
- They display photophobia (avoidance of direct sunlight)
- Odema (swelling) of the skin with warm painful swellings on the abdomen interfering with movement
- Lack of appetite, nasal discharge, diarrhoea and enlargement of superficial lymph nodes.
- Inflammation of the testicles and sterility may occur in bulls.
- Small cyst like structures may appear in the whites of the eyes. These are considered to be diagnostic.
- Up to 10% of affected animals die in the early stage.
Stage 2:
- Survivors develop a chronic disease in which the parasites are in cysts underneath the skin. These cysts contain thousands of parasites.
- The skin becomes hard, thickened and wrinkled and the hair may fall out.
- Denuded areas of skin become scurfy, cracked, secondarily infected and fly-blown.
- Death occurs in severe cases.
- Recovered animals remain permanent carriers of cysts which contain numerous parasites.
- Cysts may develop in the eyes.
- Chronic damage and calcification of the testicles may occur.
- Severely affected animals become emaciated and bulls permanently sterile.
- Goats have lumps in their ears and around the genitals. They have white patches on their eyes.
- Pregnant goats abort and many become infertile. New-born goats are weak and some die.
The early stage of the disease can be confused with Malignant Catarrh. The later stages must be differentiated from skin conditions such as Lumpy Skin Disease, Photosensitization, Streptothricosis, Mange and Sweating Sickness.
Prevention and Control
- Separate sick animals from healthy ones.
- Control flies and ticks
- A live tissue culture vaccine has been developed in South Africa which gives good results, although it does not prevent infection.
Treatment
There is no specific therapy but treatment of symptoms may be applied. Oxytetracycline appears to have some effect if given in the early stages of the disease.
Fly Strike
Fly Strike is also known as Myiasis.
There are two types of Fly strike.
There are two types of Fly strike.
1. One is caused by opportunistic fly larvae i.e. those which are usually free living but when the opportunity arises can adapt themselves to a parasitic dependence on a host. These include house flies, blow flies and flesh flies.
2. The other is caused by obligatory fly larvae, which are completely dependent on a host in order to complete their life cycle and without which they would die. These include the New World Screwworm Fly and the Old World Screwworm Fly, which is found in Africa. Screwworms are so called because the larvae have a "wood screw" shape. Screwworms tend to target cattle.
All animals get Fly Strike but sheep get it worst and most often, usually due to attack by opportunistic fly larvae. Humans are sometimes affected by fly strike.
Mode of spread
Adult flies are attracted to moist wounds, skin lesions or a soiled hair coat. Young animals with softer skin and sheep with skin folding or wrinkling around the thighs, back or tail are susceptible. Castration wounds, docking wounds and wounds around the head are favoured sites for fly strike.
Eggs, usually laid below the tips of the fleece, hatch within 24 hours if conditions are moist. Warm, humid weather favours fly strike and by far the most common site affected is the breech, because of soiling and irritation of the skin by urine in this area. Moisture, and nutrients from serum, faeces etc are necessary for survival of first stage larvae.
Opportunistic larvae move over the skin surface, ingesting dead cells, exudate secretions and debris, but not live tissue. The larvae irritate, injure and kill successive layers of skin and produce exudates. The maggots can then tunnel through the thinned top layer of the skin and go deeper, producing tissue cavities in the skin which may be several centimeters in diameter.
Advanced wounds may contain several thousand maggots and the animal may die of shock, toxaemia and infection.
Second stage larvae can scrape the skin with their mouth hooks to obtain food. Once established, Fly Strikes can spread rapidly and attract more flies. Mild Strikes can cause rapid loss of condition. Bad Strikes can cause death from shock, toxaemia or infection.
Signs of Fly strike
- Affected animals become depressed, stand with their heads down, do not feed, and attempt to bite the infested areas.
- Sheep are restless, wriggle their tails continuously and move about from place to place.
- There may be an obvious smell.
- The wool may be lifted slightly above the surrounding wool.
- The affected wool is moist and usually brown in colour.
- In the early stages larvae may be found in pockets in the wool before they have reached the skin.
Prevention and control
Prevention is by clipping the wool around the crutch, docking the tails of lambs to lessen faecal contamination, controlling scouring and reduction in fly numbers by burying carcasses and destruction of fly breeding areas, and the application of insecticides and larvaecides to the skin or fleece by dipping or jetting. All skin wounds should be promptly treated and the wool clipped away from the affected area.
Screwworms have been controlled in a number of countries by the release of irradiated sterile male flies. The female mates only once, and when mated with a sterile male lays eggs that do not hatch. The sterile males are able to mate and the release of sufficient sterile males in an area will lead to eradication.
Treatment
Treatment involves killing the larvae in the skin lesions, clipping the hair or wool, removing as many larvae as possible, applying an insecticide to kill larvae and to prevent secondary re-infestation, treating wounds promptly and effectively and providing an environment hostile to flies.
Ivermectin at dosages of 50, 100 and 300 micrograms per kg to infested cattle resulted in 100% larval mortality for at least 6, 12 and 14 days respectively.
Horn Cancer
This disease is a cancer of the base of the horn of Zebu cattle, mainly in castrated adult males, and occasionally in cows and bulls. The disease primarily affects short-horned Hariana cattle of India, and the disease is largely confined to India, but the condition has been reported in other Zebu breeds in other parts of the world. A similar condition occurs in Sudanese cattle. The exact cause of horn cancer is not known, but may be partly hormonal due to its high prevalence in adult castrates.
Affected animals commonly have a previous history of injury to the horn, or persistent rubbing of the tissues round the base of the horn from head ropes or from paring or polishing the external layers of horn. It is not an infection, but castrated males get it more often.
The type of cancer is a Squamous Cell Carcinoma.
Signs of Horn Cancer
- The earliest sign is a slight drooping of the horn at its base. This deformity increases until the horn bends downwards and becomes loose. It then becomes detached from the skin at the base, exposing the horn core
- A grey/yellow lump can be seen at the base of the horn. It is covered with blood and mucus; it smells bad and is often infected
- The cancer has cauliflower-like growths covered in foul-smelling blood -stained discharge
- It may invade the frontal sinuses causing discharges with pus from the nose
- Often there is involvement of the eye, with cloudiness of the eye
- The cancer may spread inside the animal to other parts of the body. If left untreated, the animal becomes distressed and unhealthy
- Bacterial infection or Blowfly Strike may be complications
Control and treatment
- Early cases may respond to surgical removal provided there has been no invasion of internal organs
- Irrigation of the frontal sinus with acid-pepsin solution may be advantageous
- Dehorning of young long-horned animals, particularly those with a familial history of horn cancer, is probably the most reliable measures
Lumpy Skin Disease (LSD) and Pseudo-lumpy Skin Disease (PLSD)
LSD is an infection of cattle only believed to be transmitted by biting insects and caused by a poxvirus closely related to that which causes Sheep and Goat Pox. It is different from Pseudo-lumpy skin disease (PLSD), a benign and harmless but completely separate disease caused by a herpes virus.
LSD
The disease is endemic in sub-Saharan Africa and Madagascar and has spread to Egypt and Israel. It is believed to be insect-borne, but the exact insect responsible is at present not known. Buffalo may act as carriers and contact infection may also occur.
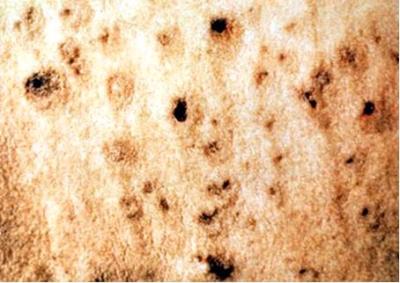
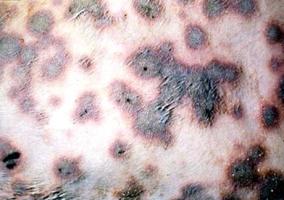
Signs of LSD
|
|
|
|||||||||
|
|
|
- Animals may salivate profusely. A clear discharge comes from the eyes and nose. Later the discharge from the nose becomes grayish/white.
- The cattle are weak and tired and stop eating. They have a fever that sometimes goes down after 1 - 2 days but it goes up again. Animals produce little milk and pregnant cattle often abort.
- Lumps appear on the body, usually around the head and neck, under the abdomen, on the legs, or around the genitals and the udder. Sometimes the whole body is covered in lumps.
- The lumps are hard and usually all are about the same size- from 0.5 to 5.0cms in diameter. The hair on the lumps stands up. The lumps are located within the skin and are firm, raised, round and flattened. Softer, yellowish/grey lumps may appear on the mouth. They rub off easily leaving sore red patches.
- The lymph nodes enlarge and sometimes a leg swells with persistent, painful oedema, accompanied by sloughing of the skin, leaving a large, open suppurating wound. Scars may be left which damage the hide. Healing may take several weeks, and hardened lumps may remain.
- The nodules dry and slowly begin to separate from the surrounding skin, finally sloughing, leaving an unsightly ulcer, which slowly heals, leaving behind a damaging scar.
- Adult cattle do not usually die but they may take months to recover and a few of them become very thin.
- Young calves often die.
- Occasionally the disease is very mild; animals only have a low fever and lumps in the skin that heal in about six weeks.
- Sometimes nodules spread to the upper respiratory tract, causing difficulty in breathing, and death within 10 days.
- Sometimes many animals are affected, sometimes only a few. Of those affected, some animals are very ill and may die. Others are only mildly ill. Yet others may take a long time to recover, and remain in poor condition for weeks. Pregnant cows may abort.
The sudden appearance of lumps in the skin after an initial fever, with sometimes rapid spread to other animals make it difficult to confuse Lumpy Skin Disease with any other disease. The only other disease which might cause confusion - Pseudo-lumpy Skin Disease (PLSD) - is only seen on the outside layers of the skin, or confined to the teats.
PLSD
The PLSD virus primarily causes Bovine Ulcerative Mammillitis, a severe, ulcerative condition of the teats and udder of cows, mostly newly calved dairy heifers, but also previously unexposed cows. Biting insects are believed to initiate infection.
Signs of PLSD:
- PLSD, like true LSD, causes circular or oval plaques in the skin that are about 1cm in diameter, are hard and firm and have a red edge.
- Over the next few days the plaques enlarge to a diameter of 3-5cm. Their centres are depressed, discharge and form a thin brown crust.
- The skin beneath the crust dies and peels off 2 weeks later, leaving a bald patch of new skin covered with fine, grey scales. New hair covers the area within 2 months
- The number of plaques ranges from a few to many and they may be found anywhere on the skin, but mostly on the face, neck, back and perineum.
This condition is endemic in Eastern and Southern Africa and the US. This is a benign disease for which treatment is not warranted and is often missed. Its importance lies in its superficial similarity to true Lumpy Skin Disease.
LSD Mode of spread
Outbreaks of true Lumpy Skin Disease often occur at the start of the rains. Although biting insects are believed to be mainly responsible for transmission, contact infection via infected saliva is also accepted as a method of spread.
Known sources of infection include permanent swamps, from where new outbreaks may start. Outbreaks may be small and isolated or gradually spread to cover large areas of the country and even spread into neighbouring countries, affecting thousands of animals. Imported breeds of cattle appear to be more susceptible than local breeds. The disease may be confused with besnoitosis, dermatophilosis, or ringworm.
The incubation period ranges from 2 to 4 weeks. The disease may be peracute (very rapid onset), acute (rapid onset) or inapparent. All ages are affected.
Prevention and control
Vaccination for Lumpy Skin Disease is effective. Vaccinate all animals in contact with the disease. Preventive vaccination is also advisable using the modified sheep/goat pox vaccine made by KEVEVAPI in Nairobi.
PLSD is of relative insignificance other than that it can confuse the diagnosis of the much more significant LSD.
Recommended treatment
There is no specific treatment for Lumpy Skin Disease but the prevention of secondary infection is vital, using antibiotics and sulphonamides.
Orf
 |
| Orf Symptoms |
| © Hugh Cran, Nakuru, Kenya |
Common names: contagious pustular dermatitis
Description: Viral skin disease
| WARNING: Notifiable disease! If you suspect an animal has Orf, you must inform the authorities immediately. |
Orf is an infectious viral skin disease of mainly sheep and goats. It mainly affects the lips of young animals. The disease is more severe in goats than in sheep. It can also affect wild sheep and goats. Humans are occasionally infected and the disease has been reported in dogs that have scavenged on infected carcases.
It is characterised by the development of pus-filled and scabby wounds on the muzzle and lips of lambs and kids, by the appearance of similar lesions on the teats of nursing ewes and nanny goats and it can also produce lesions on the teats of cows.
The cause is a pox virus related to that which causes Pseudo Cow Pox and Bovine Papular Stomatitis. The disease occurs worldwide. It occurs mainly in young lambs and kids and occasionally in mature animals which do not have immunity from natural exposure.
Mode of spread
This is probably the most common viral disease of sheep. It is spread by contact. The source of new outbreaks in sucking lambs is believed to be a flare up of a persistent infection in a stressed ewe following lambing, not, as was previously thought, from scabs lying on the pasture. The virus then spreads rapidly to other lambs in the flock, both directly and indirectly. The incidence within a flock may be as high as 90%. The few deaths which occur are the result of extension of wounds within the respiratory tract, but the mortality rate may reach 15% if the lambs are badly cared for or if secondary infection or fly strike occurs.
Epidemics tend to occur twice yearly - the first peak is associated with the disease in sucking lambs, the later one with susceptible stock lambs. But sporadic cases can occur at any time.
The disease is commonest in lambs aged 3-6 months, although lambs aged 10-12 days and adults can be severely affected. Outbreaks can occur at any time but are most common in dry conditions. Recovered animals are solidly immune for 2-3 years but they do not transfer this immunity in their colostrum to their lambs, which are therefore susceptible to infection.
In humans typical wounds occur at the site of infection, usually an abrasion infected while handling diseased sheep, or milking infected cows or by accidental means when vaccinating sheep. The lesions are very itchy and respond poorly to treatment.
Infection only occurs if there is a break in the surface of the skin or the lips. The rapid spread during dry conditions may be due to scratches on the skin caused by dry feed, allowing a ready entry of infection. Spread in a flock is very rapid and occurs by contact with other infected animals or non-living objects. Ewes nursing affected lambs often develop crops of lesions on their teats which sometime lead to mastitis. As a result lambs are unable to suckle and may suffer from starvation.
|
Signs of Orf
Diagnosis The wounds are characteristic. However they must be differentiated from those of viral Ulcerative Dermatosis, which destroys tissue and causes ulcers around the nose, mouth, legs and on the penis, prepuce and vulva of older sheep. It must also be differentiated from Strawberry Foot Rot, caused by the fungal organism dermatophilus cogolensis, which usually occurs on the lower limbs, from Bluetongue and from Sheep and Goat Pox.
Treatment There is no specific treatment. Antibiotics may help to combat secondary infections, and soft palatable food should be provided.
People should exercise caution when handling infected sheep, as lesions, usually confined to the head or face, can spread at a rapid rate and be distressing.
|
|
Prevention and Control
In the early stages of an outbreak, affected animals should be isolated and the remainder vaccinated. Vaccination is of little value when a large number of animals are already infected.
Persistence of the disease in a flock is common and in such circumstances the lambs should be vaccinated when about 1 month old. A small amount of live vaccine is brushed over light scarification of the skin, usually on the inside of the thigh.
For best results a second vaccination about 2-3 months later is suggested.
A week after vaccination there should be a local reaction with the formation of scabs at the site of vaccination and vaccinated animals should be segregated from unprotected stock until the scabs have fallen off.
Sheep that have recovered from natural infection are highly resistant to re-infection and vaccination is completely effective for at least 2 years.
Photosensitization
|
Photosensitization is a condition in which areas of skin exposed to light and lacking sufficient protective hair, wool or pigmentation, are very sensitive to sunlight due to the presence of chemicals called photodynamic agents.
Photodynamic agents (or photosensitizing substances) are activated by light, and may either be in something the animal eats (and cause primary photosensitization) or be formed in the animal's body due to faulty excretion through the liver (and cause secondary photosensitization).
Many chemicals, including some that are fungal and bacterial in origin, may act as photosensitizing agents. However, most are from plants.
The condition occurs world-wide and is most commonly seen in cattle, sheep, goats and horses.
Primary photosensitization occurs when the photodynamic agent is absorbed either through the skin or the gastrointestinal tract unchanged, and reaches the skin in its original form. Livestock are usually affected within a few days of eating the plant when it is lush and green and growing rapidly. In most cases the plant responsible must be eaten in large amounts and is usually the dominant plant in the pasture.
|
|
Examples of plants causing primary photosensitization include St. John's Wort, buckwheat, wild carrot, perennial rye grass, certain species of clover and lucerne and spring parsley. In addition some coal tar derivatives, phenothiazine, sulphonamides, and tetracyclines have induced primary photosensitization.
Secondary photosensitization is by far the most common form seen in livestock. The photosensitizing agent is in all cases phylloerythrin which is a normal end-product of plant chlorophyll excreted by the liver. When the liver is not functioning properly and fails to excrete it, pylloreythrin accumulates in the blood and may reach levels in the skin which make it sensitive to light.
A number of plants contain liver poisons that may result in secondary photosensitization if eaten in sufficient quantities, including:
1. Lantana camara, ornamental garden shrubs, which have become wild in many parts of the world and are now found throughout sub Saharan Africa. Lantana poisoning is virtually confined to cattle.
2. Tribulus terrestris/devil's thorn is a ground creeping plant with yellow flowers widespread throughout the tropics; it is regularly eaten by livestock without causing problems, but is also suspected to cause photosensitization.
Numerous other plants including ragwort, lupin, bog asphodel, panic and millet grasses may also cause secondary photosensitization, as may various fungi contaminating several species of grass.
Photosensitization also occurs as a result of poisoning or infections which damage the liver. Infections include Leptospirosis in which the initial infection is in many cases followed by severe jaundice and photosensitization.
|
|
Signs of photosensitization
Regardless of the cause the symptoms are similar in all cases.
- Only pale areas not covered by a heavy coat of hair or wool are affected. Light on these sensitive areas causes swelling and intense irritation. The difference between affected and normal skin is usually very marked. Black skin is unaffected while white skin is targeted. Loss of skin is common in the terminal stages.
- The skin wounds are most common in those areas exposed to solar rays, such as the back, the flanks, nose, the vulva and the teats.
- Often the first sign is a cow stamping her feet in discomfort. The teats appear reddish and are very tender. The muzzle and vulva may appear to be swollen and peeling.
- White skin may feel dry and have the feeling of parchment while adjacent black skin feels smooth and soft.
- Affected animals seek shade and may rub the affected parts on bushes and posts.
- With time the affected skin dies, dries and peels off. It should never be pulled off.
- Usually affected animals are not ill, although on occasion they can be, depending on the cause of the photosensitization.
- If there is severe liver damage the mucous membranes may sometimes become yellow.
Prevention - Control - Treatment
- General treatment includes immediate removal from direct sunlight, removal from the paddock in which the animals have been grazing and the administration of laxatives such as liquid paraffin to eliminate toxic materials already eaten.
- Some plants are only poisonous at certain times and the pasture may be safe to return to later in the year.
- Remove known poisonous plants in pastures by digging or burning out.
Treatment of the wounds depends on their stage. Antihistamines should be given immediately. Corticosteroids, given in the early stages may be helpful, but must NEVER be given to pregnant animals as it will make them abort
.
Secondary skin infections and suppurations should be treated with basic wound management and Fly Strike prevented.
Most wounds heal remarkably well, even after serious infection.
Pox Diseases
|
Most pox diseases occur in Africa and Asia. Sheep and goat pox occurs in Africa north of the equator and in Asia.
Pox diseases are viral diseases which affect many animals, including humans and birds but not dogs. Different species of animals are affected by different pox diseases: camels are affected by Camel Pox, Sheep and Goats by Sheep Pox and Goat Pox, Pigs by Swine Pox, poultry by Fowl Pox and cattle by Cow Pox and Psuedo-cow Pox.
|
|
Sheep pox symptoms
Infection may be followed by wounds all over the body (e.g. Sheep Pox) or in one area (e.g. Pseudo- Cow Pox). Some strains of pox virus with reduced virulence are used to immunize against some infections, the classic example being the global eradication of smallpox in humans by immunization with strains of live vaccinia virus, which is a laboratory generated virus related to Cow Pox.
Other diseases which cause skin lesions can be confused with pox infections e.g. Bluetongue, Foot and Mouth Disease, Mange and Contagious Pustular Dermatitis (Orf).
Mode of spread Infection is acquired either by inhalation or through the skin. In certain instances the virus is transmitted by biting insects (e.g. Fowl Pox and Swine Pox).
|
|
Cow Pox
True Cow Pox is a rare disease. The vaccinia virus previously used to vaccinate humans against Small Pox was in many instances responsible for explosive outbreaks in cows as infections closely mimic cow pox. In cattle, cow pox is a relatively benign disease affecting the teats of lactating cows. However the virus which causes cow pox can affect cats, appearing first as a wound around the head followed by wounds elsewhere on the body.
Cases of Cow Pox/Cat Pox have only been authenticated in Western Europe. Vaccinia outbreaks in cattle however have been common when people were being vaccinated against Small Pox. More humans have probably been infected by Cow Pox/Cat Pox than cows.
Signs of Cow Pox
- Cattle become sick 5 - 10 days after they get infected
- They have small red sores on the teats at places where there are small injuries. The sores soon have scabs over them. When the scabs fall off they leave a crescent of smaller scabs.
- The teats become rough with many grayish/yellowish scabs.
- In cats a single pock is followed by the appearance of multiple widespread wounds
- Animals usually recover in 2 - 8 weeks.
Pseudo-Cow Pox
is a common, mild infection of the udder and teats of cows and occurs worldwide.
Other names for Pseudo-Cow Pox include Bovine Papular Stomatis (BPS) and Milkers' Nodules.Pseudo-Cow Pox is visible as eroded patches on the teats and udders of lactating cows, whereas BPS is acquired by calves suckling cows with active Pseudo-Cow Pox and is visible as circular patches around the nose and mouth and by a pimple-like inflammation on the margins of the nostrils, inner surfaces of the lips, and the edges of the tooth sockets.
| ATTENTION: Human beings can be infected with BPS and the disease in humans is called Milkers' Nodules. |
Pseudo-Cow Pox mode of spread
Calves are infected when they suck the teats of infected cows. They in turn infect in-contact susceptible calves by licking. Thereafter the virus becomes inactive and resurfaces whenever there is stress. It is suspected that the first case in a dairy herd is a resurfaced infection in a cow originally infected as a calf. Thereafter, the virus is spread to the teats of other milking cows by the hands of milkers, cloths, by contact and via teat cups.
Signs of Pseudo-Cow Pox
- Lesions begin as small, red pimples on the teats or udder. These may be followed rapidly by scabbing or small blisters may develop before scabs form.
- Scabs may be abundant but can be removed without causing pain.
- As the lesion begins to heal, it becomes raised, healing from the centre, and leaves a circular ring of small scabs. This stage is reached in 7-12 days.
- Some wounds persist for several months giving the affected teats a rough feel and appearance. There is little immunity and the disease tends to recur. It spreads slowly, heals slowly, recurs cyclically in individual cows, and in herds the disease can last for up to 18 months.
Signs of Pseudo cow pox in calves (Bovine Papular Stomatitis)
- Calves show signs 3-7 days after they are infected
- The pimples increase in size daily until they are 1-2cm in diameter.
- The initial wounds persist for 3-4 weeks and then heal quickly, to be followed by new wounds 1-3 weeks after the onset of the first ones.
- The wounds expand, forming circles of different colours - yellow, grey and red.
- As old wounds heal, new ones may form, so the disease may be protracted for months.
- Animals are not ill and the disease is not fatal.
- Occasionally the tip of the tail may be affected, leaving a raw, denuded area. Infected animals are chronically unthrifty and are usually culled. The condition is called 'Rat Tail Syndrome'.
Prevention and Control
- Infected animals should be segregated. Avoid moving infected animals to areas without the disease.
- Individual paper towels should be used for washing udders.
- Back-flush milking clusters to reduce cross-infection
- Newly purchased cattle should be quarantined for at least 14 days and their teats carefully inspected for evidence of infection.
- Control by vaccination has been attempted but is of doubtful value.
- Avoid using anything that has touched infected animals.
- Make sure that newborn animals drink enough colostrum.
- Those people who milk infected animals should not milk healthy ones. It is best not to drink milk from infected animals.
Recommended treatment
- Only treatment of symptoms without curing the disease is possible. The application of a soft cream before milking and an astringent lotion after milking facilitates recovery. Hands and cloths should be disinfected.
- If the sores are bad or deep put antibiotic or antiseptic on them. Be careful not to spread the disease further. Use wound dressings that dry.
Camel Pox:
Camel Pox is a malignant pox of camels, characterized by fever, skin wounds all over the body and a low, but significant death rate. Spread is both direct and indirect. In fatal cases, the head is most often affected, with lesions concentrated around the eyes, often blinding the animals. In addition there is widespread facial swelling.
A vaccine for camel pox exist, but has so far been too expensive to import to Kenya.
A vaccine for camel pox exist, but has so far been too expensive to import to Kenya.
|
|
Sheep and Camel Pox:
These are serious and often fatal diseases characterized by widespread skin eruptions. Fever and a variable degree of systemic disturbance develop. Eyelids become swollen and a mucous discharge with pus encrusts the nostrils. Widespread skin wounds develop that are most readily seen on the muzzle, ears and areas free of hair and wool. In severe cases wounds develop in the lungs. Transmission may be by direct contact, by biting flies or be airborne.
Prevention and Control: Live, attenuated virus vaccines give good immunity. |
Pigs:
All ages may be affected but Swine Pox is most often seen in young pigs 3 - 6 weeks old. Transmission is generally via stable flies or the biting louse.
Ringworm
Ringworm is a fungal infection of the skin of all domestic animals (cattle, horses, mules, donkeys, pigs, dogs, cats and camels) and humans. It is NOT a worm infection!
It is caused by Trichophyton and Microsporum spp. The disease occurs worldwide.
Mode of spread
The infection is spread by direct or indirect contact. Licking with the tongue spreads the fungus.
Spores of the fungi can survive for prolonged periods off the host, however, and infection can arise from contact with contaminated stalls, ropes, utensils, etc.
Spores can also survive on animals without necessarily causing disease and such "carrier" animals are another source of infection.
It is more common where animals are housed or kept in close proximity to one another. A high humidity is known to be conducive to multiplication of the fungus. Animal susceptibility is largely determined by immunological status so young animals are most susceptible. Nutritional status may play a part, as may dietary deficiencies.
Transmission between species readily occurs and in rural areas 80% of cases of human ringworm are derived from animals.
Ringworm fungi only grow in keratinized tissue and advancing infection stops on reaching living cells or inflamed tissue. The fungi require oxygen and die out in the centre of the lesion leaving only the edge active. It is this mode of growth which produces the characteristic ring form of the lesions.
Generally speaking the disease is minor in its effect on the affected animal and little economic loss is incurred.
Zebu breeds appear to be less commonly affected than European breeds.
Sings of Ringworm
- Animals develop symptoms of ringworm 7 - 28 days after infection.
- Animals have a circular scab on the skin about 3 cm across. Scabs usually appear first around the nose, above and around the eyes, on the ears or under the tail. The skin under the dry scab is wet. Scabs soon join together and become thicker.
- After several days the scabs fall off. The skin underneath becomes dry with a heavy, gray-white crust raised above the skin.
- Animals do not scratch when they have ringworm. But they sometimes scratch if bacteria infect the scabs.
- The scabs fall off after a few weeks and leave patches with no hair.
- Animals slowly recover even without treatment. The hair grows back in about three months.
Prevention and control
- Isolate and treat animals with ringworm
- Failure to control an outbreak of ringworm is usually due to the widespread contamination of the environment before treatment is attempted.
- Use disinfectants to clean contaminated places and equipment before using them for healthy animals. Direct sunlight kills ringworm fungi.
- An attenuated fungal vaccine is available in some European countries and it has prevented the development of severe clinical lesions and greatly reduced the incidence of zoonotic disease in animal care workers. But vaccinated animals continue to shed spores for some time after vaccination and it is expensive.
- Animals that recover from ringworm do not usually get the disease again.
Treatment
Animals usually recover spontaneously from ringworm with no treatment but it may take 2 - 3 months. They recover sooner when it is dry and sunny. The main advantage of any treatment is to prevent the extension of recent lesions and to limit the spread of infective material. Treatment greatly reduces contamination of the environment and as such is to be encouraged. To help recovery:
- Shave the hair around the place with ringworm. Burn the hair you have shaved off because it is infected.
- Scrape the scabs off gently using soapy water and a brush.
- Put antiseptic on the affected areas. Betadine povidone- iodine, Whitfield's ointment and chlorhexadine are effective. Animals treated like this can recover in 2 - 3 weeks.
- Give griseofulvin by mouth or apply to the affected area. Individual animals can be treated with miconazole or clotrimazole lotions. These medicines are expensive but animals treated with them start to recover in about 10 days
Common traditional practices
- Kipsigis (cattle): Crush a handful of Mexican marigold (stem, leaves and flowers) with a stone so the juice comes out. Collect the juice and rub on the affected spots once a day for 3 days.
- Luo (camels, cattle, donkeys, goats, sheep): Pound a handful of Otange leaves to powder and mix with half a cup of ghee. Smear on the affected skin until the patches disappear.
Skin Tumours and Warts
|
All domestic animals can get skin tumours. Humans are not affected by skin tumours from animals.
Some viruses e.g. the papilloma virus, may cause skin tumours.
There are two types of skin tumours: benign (warts) and malignant (skin cancer). Benign tumours are not life-threatening, do not spread to other areas of the body and either regress or are amenable to treatment and generally grow slowly. Malignant tumours can be life-threatening, grow quickly, can spread to other organs or tissues and may be difficult to treat.
In cattle, warts commonly are found on the head, neck and shoulders, and occasionally on the back and abdomen. One form appears on the teats in older animals. Warts appear about 2 months after exposure to the causal virus and may last for up to or longer than a year.
Apart from warts, the other most common skin tumour found in cattle is the Squamous Cell Carcinoma. This is a malignant tumour most commonly seen affecting the eye, the vulva or, less commonly, the back, of light skinned European breeds. It grows quickly, does not disappear but grows larger, smells, and requires urgent veterinary attention. If one of these is suspected do not wait, but call a vet. It will not go away!
Mode of spread of Warts Spread is generally by direct contact with infected animals. Papillomatosis may become a herd problem when a large group of young susceptible cattle become infected. Most of these warts look like a cauliflower. Another type, which is flatter with a warty surface, may involve the venereal regions, where they can cause pain, disfigurement, infection of the penis of young bulls and difficulty in calving when the vaginal mucosa of heifers is affected.
Immunity after recovery is solid and persists for at least 2 years. The lack of susceptibility of adults to natural infection is thought to be due to immunity acquired by apparent or unapparent infection when young.
|
|
Signs of Skin Tumours
- Hard lumps on the skin that are not hot are often tumours. These lumps may grow slowly, in which case they may be benign. If they grow fast they are probably malignant. Sometimes the skin over a tumour is injured and the lump has open sores on it. If this is the case the tumour is most probably malignant. It is better to get a professional to examine it early than to wait until it is too late to do anything about it.
Horses, mules and donkeys sometimes get skin tumours called Sarcoids. These are the most frequently recognized tumours of horses. A virus, probably the bovine papilloma virus, is suspected. They can be transmitted by direct or indirect contact or by insects. They can grow anywhere on the body but the base of the ear, on the penis, around the eyes and low on the legs are favoured sites. They do not normally spread through the body but they often grow back if they are surgically removed. Treatments are available.
Young horses often get small scattered papillomas on the nose, lips, eyelids, lower legs, penis, vulva, mammary glands and inner surface of the ears, often following mild scratches. They can be a herd problem especially when young horses are run together, but regress in a few months as the foal's immune system matures. When they develop in older horses they can persist for more than a year.
Camels about a year old can get small skin tumours around the lips and nose. Older camels sometimes get tumours, especially on the teats. The tumors disappear on their own after a few months.
Prevention - Control - Treatment
- There is no known treatment for most tumours. Some tumours do not spread to other parts of the body (these are the benign tumours). Skilled veterinarians sometimes remove benign tumours. Some tumours spread to other parts of the body (these are the malignant tumours). It is not worth operating to remove these because they come back in other parts of the body.
- Infectious papillomatosis disappears on its own, although the duration of warts varies considerably. A variety of treatments has been advocated without agreement on efficacy. Surgical removal by a vet is recommended if the warts are sufficiently objectionable. However, because surgery in the early growing stage of warts may lead to recurrence and stimulation of growth they should be removed when near their maximum size.
- Affected animals may be isolated from others likely to be infected, but with the long incubation period many are likely to have been exposed before the problem is recognized.
- Vaccines are of some value for prevention but are of little value in treating cattle that already have lesions. Because wart viruses are mostly species specific there is no merit in using a vaccine derived from one species in another.
- When the disease is a herd problem it can be controlled by vaccination with a suspension of ground up wart tissue in which the virus has been killed by formalin. An autogenous vaccine i.e. one derived from animals in the affected herd, may be more effective than a commercial one.
- The best action is to do nothing yourself, but call a veterinarian to assess the problem. Trying to treat a tumour without knowing its type may lead to disaster! Leave well alone and call a vet.
Worm Nodules Disease
Worm Nodule Disease is an infestation of the skin of cattle, horses, and camels with small, long (up to 60mm), slender Onchocerca worms. The disease occurs worldwide, but is more common in the tropics and sub-tropics. In livestock, infestations are rarely a problem but it may be necessary to differentiate them from other more serious skin diseases such as Mange and Skin Tuberculosis. The wounds in the skin contain the microscopic larvae of the worms, called microfilariae. Midges and small biting black flies ingest the microfilariae, which develop into infectious larvae in the flies. The flies then pass the infection to another host when feeding. The infectious larvae migrate to the place where nodules develop and adult females produce microfilariae.
Signs of Worm Nodule Disease
- Clinical signs are minimal, consisting of nodules up to 3cm in diameter under the skin and internally. In cattle skin nodules are found in the brisket, lower limbs and ligaments of the neck whereas in horses they are found in the ligaments of the neck and lower limbs.
- Animals have small lumps (called nodules) just under the skin. The lumps are full of worms and worm larvae.
- Cattle usually have lumps on the legs, around the genitals, on the neck and between the front legs.
Diagnosis
Skilled vets can check a piece from one of the lumps for these worms with a microscope. The microfilariae can be easily seen in biopsies of nodules examined under the microscope.
Prevention - Control - Treatment
- Ivermectin works well against the microfilariae. Other medicines are less effective.
- Control of the vectors is usually impracticable.
Two other species of worm affect the skin of cattle:
Parafilaria bovicola occurs in the subcutaneous tissue (beneath the skin) and is carried there by face flies. Mature female worms puncture the skin to lay eggs on the surface and there is a heavy discharge from the wounds. The inflammation and swelling at the sites of infection resemble subcutaneous bruising and such areas have to be trimmed off at meat inspection and the hides downgraded
.
Ivermectin is effective as a treatment.
Rhabditis bovis is a worm which normally lives in the soil, but has become adapted to living in the ears of cattle in East and Central Africa. Signs include a putrid discharge from the ear, continual wasting, and a severe drop in milk yield. Central nervous signs and death may result.
Treatment of affected cattle with Ivermectin is effective.
Wounds and Abscesses
Wounds/Definition
The word "wound" is taken to mean any break in the skin or mucous membrane. The underlying tissue is frequently also involved. Wounds occur in all animals on every farm and arise from a variety of causes.
Wounds may be classified in various ways. For example they may be described according to their site - wounds of the neck, head, chest, abdomen or limbs. Another classification may indicate their particular type - for example crushing, lacerating or penetrating wounds, bites by other animals, snakes or insects etc, cuts or burns. Wounds may be fresh, bleeding, infected, gangrenous or swollen.
Some wounds may be small and insignificant. Others may be large and even life threatening, especially if they involve major blood vessels.
Such descriptions are very important when describing the nature of a wound to a veterinarian who then should be in a position to offer useful advice even if he, or she, is unable to attend personally to the case.
What to do about Wounds
It is best to assume that all wounds are potentially infected and to treat them as such, irrespective of their cause, site or nature.
Large, deep wounds requiring suturing are best dealt with by a veterinarian but the layperson can do much either to make things easier until the arrival of a qualified person or to treat smaller wounds without outside assistance.
Prevention of infection
Prevention of Infection is important. Contamination of wounds may lead to severe generalized disease such as gas gangrene, tetanus etc as the bacteria which cause such diseases live in the soil or even in the buildings where animals are housed.
The most important principle in the care of fresh wounds is to maintain the viability and the defensive mechanisms of the tissues, so that they may play a part, unweakened, in the healing process.
All harmful influences must be avoided during and after treatment.
All harmful influences must be avoided during and after treatment.
All instruments and utensils and dressing must be scrupulously clean before use. Hands must be washed and scrubbed.
Some of the common disinfectants that can be used in wound treatment include:
1. Hydrogen peroxide (painless) - apply undiluted
2. Spirit
3. Dettol (stings) - dilute
4. Savlon (painless) - dilute
5. Iodine (minor stinging) - according to recommendation on bottle
6. Potassium permanganate - dissolve granules in water
7. Epsom salt - dissolve in warm water
8. Table salt (less effective) - dissolve in warm water
9. Warm Soap water
10. Magadi soda (mostly used to treat wounds from Foot and Mouth disease)
2. Spirit
3. Dettol (stings) - dilute
4. Savlon (painless) - dilute
5. Iodine (minor stinging) - according to recommendation on bottle
6. Potassium permanganate - dissolve granules in water
7. Epsom salt - dissolve in warm water
8. Table salt (less effective) - dissolve in warm water
9. Warm Soap water
10. Magadi soda (mostly used to treat wounds from Foot and Mouth disease)
Bleeding wounds
If there is bleeding this must be stopped. Unless the bleeding is very severe as from a large severed blood vessel then firm pressure with a pad of dry cloth, towel or large wad of cotton wool over a period of several minutes should in time stop the bleeding.
If this pressure is not sufficient and the bleeding continues and begins to weaken the animal then a tourniquet may be applied. This is a firm band applied and tied a few inches away from the wound on the side nearest to the heart. This may be made from anything that is strong and long enough - a bandage, a handkerchief, a rope, a piece of inner tubing etc. With any tourniquet the pressure should be maintained for a few minutes after the bleeding has stopped but it should never ever be tied for longer than necessary and never longer than 15 minutes or so.
Once the bleeding has stopped wait for a few more minutes. Then carefully shave the edges of the wound for about 2-3 inches all round. Then clean the edges with antiseptic or spirit. If there is foreign material in the wound such as dirt, grass, glass, grit, dung, this should be carefully removed and the wound washed out with salty or clean water. Instill antibiotic ointment in the form of a tube of intramammary ointment into the wound or sprinkle it with antibiotic powder.
Large gaping wounds
If the wound is a gaping one then it will be necessary to join the edges together with stitches to accelerate healing. This may be done with nylon sutures, or with thick sewing-cotton or thin tape if nylon is unavailable.
All material to be used should be boiled before use and the operator's hands must be scrubbed clean and disinfected.
The injection of local anaesthetic along the edges of the wound will greatly ease the insertion of stitches and is obviously more humane.
If no surgical needle is available then a large-eyed sewing needle will serve the purpose. The stitches should be single and separate and loosely tied.
Antibiotic should be given after the wound has been treated.
If healing does not proceed cleanly and pus appears then remove the lower stitches to allow drainage and keep the wound clean and open until healing occurs.
All wounds must be protected against flies which may lay their eggs in wounds which may then become infested with maggots.
Wounds on the lower limbs should be carefully bandaged with a firm pressure bandage after treatment and the bandages changed every 2 or 3 days to check on the progress of healing. Do not attempt to stitch wounds on the lower limbs. The stitches invariably will not hold and will tear our.
Puncture wounds:
should not be stitched, but left open to drain and cleaned and treated frequently with antibiotic either locally or by injection. All discharges of pus or serum should be washed away whenever they appear.
Closed wounds:
may result in contusions or bruises when the skin is unbroken, but there may be much damage to underlying tissues in the form of swelling, haemorrhage (internal bleeding) and tearing of muscles, tendons and ligaments. There may be considerable pain, and the area may be swollen, tense, hot and be discoloured black, red or purple.
Most bruises resolve without any special treatment but may benefit from anti-inflammatory drugs of the application of cold water, ice or in some cases by the application of a kaolin and glycerine poultice.
Some closed wounds may develop into Haematomas. These are large blood blisters which develop when there is bleeding into a pocket underneath the skin. They are not usually painful but may be quite large. If left alone they will gradually shrink as the blood inside clots and organizes and the serum is absorbed. Finally a scar will be left. To confirm that the swelling is a haematoma a large sterile needle should be pushed through the skin into the swelling when serum or blood will come out. A haematoma should not be opened immediately in case there is still seepage of blood. After a few days it can be opened. The lower part should be carefully shaved and disinfected and a line of local anaethetic injected. Then an incision should be made through the skin. Once serum starts to flow from the wound the cut can be enlarged to allow all the fluid to flow out. An injection of antibiotic should be given to prevent infection from developing.
Abscesses
An abscess is a swelling with pus usually below the skin. It must be differentiated from other swellings such as those caused by hernias, ruptures, tumours, cysts and haematomas.
Abscesses are usually hot and painful when touched, whereas ruptures, hernias, tumours, haematomas and cysts are normally non-painful. Hernias and ruptures usually occur below the belly and may contain internal organs such as a loop of intestine. Cutting a swelling like this could be disastrous. So check and think before taking action, by feeling the swelling carefully. A hernia or rupture is usually soft and can be pushed back into the body and is usually situated on the body wall.
Abscesses are usually hot and painful when touched, whereas ruptures, hernias, tumours, haematomas and cysts are normally non-painful. Hernias and ruptures usually occur below the belly and may contain internal organs such as a loop of intestine. Cutting a swelling like this could be disastrous. So check and think before taking action, by feeling the swelling carefully. A hernia or rupture is usually soft and can be pushed back into the body and is usually situated on the body wall.
An animal with an abscess may have a raised body temperature due the pus inside the abscess. Squeezing the swelling may cause pus to ooze through the skin.
In order to confirm that the swelling is an abscess a sterile needle should be carefully pushed through the skin into the swelling after first shaving the overlying skin and applying spirit or antiseptic to the site of the insertion. If the swelling is an abscess then pus will appear in the hub of the needle. If a cyst there may be clear fluid, if a haematoma serum, if a tumour then possibly nothing may appear.
In order to confirm that the swelling is an abscess a sterile needle should be carefully pushed through the skin into the swelling after first shaving the overlying skin and applying spirit or antiseptic to the site of the insertion. If the swelling is an abscess then pus will appear in the hub of the needle. If a cyst there may be clear fluid, if a haematoma serum, if a tumour then possibly nothing may appear.
Treatment of abcesses
1. Bathe the overlying skin with warm medicated water until the abscess bursts and drains. Recipe below.
2. Lancing the abcess when it is ready.
1. Mix salt or Epsom salts in water as hot as you can comfortably bear your hands in. Add a teaspoonful of salt in half a litre of water. Soak a piece of clean cloth or cotton wool with this solution and hold it on the swelling. When the cloth gets cool soak it again in the hot solution. Continue for about 5 minutes and do this at least 4 times daily.
The skin may soften and break, discharging pus, which may smell foul. Keep on bathing with the solution to encourage the drainage to continue so that no pus remains when the skin closes and heals.
If the abscess does not burst after a few days, then it may be necessary to lance it.
This is done using a scalpel or a very sharp, very clean blade as follows:
Shave the hair over the swelling and clean the area with soap and water, followed by spirit or alcohol. If you have any, inject local anaesthetic along the line of the proposed incision. Cut boldly through the skin at the lowest point to facilitate drainage. Sometimes you may have to cut quite deeply but if you saw pus draining through the needle this deep cut is necessary. Make one long vertical cut. Place a clean finger (if possible use disinfected plastic gloves) through the hole to help to release the pus which should pour out, often under pressure.
When the pus has stopped flowing, flush the cavity with a dilute solution of iodine or hydrogen peroxide solution.
Continue bathing the area with a warm salt solution for the next few days. Give an injection of antibiotic, such as long acting oxytetracycline. Healing should take place after a week or so.
Skin Symptoms as Signs of other Diseases
- Skin lesions on head, neck and shoulders with loss of hair and formation of white crust patches which are very itchy: See:
Mange (under construction) 
Mange on neck of a camel © Dr Bernard Faye 
Detail of mange on neck of camel © Dr Bernard Faye - Swollen lips with cracks that form scabs around the mouth of kids and lambs: See: Orf
- Many lumps in a line along the legs: See: Bovine Farcy
- Dry skin, black area high on the leg with crackling sound when handled: See: Black Quarter (under construction)
- Blisters in cow's mouth and sores between the cow's toes; blisters in the teats: See Foot and Mouth Disease
- Profuse, moist eczema and hyperemia of skin and visible mucus membranes; matted hair and tips of ears; tail sloughing off: see: Sweating Sickness
Review Process
2. Hugh Cran , Practicing Veterinarian Nakuru. March - Oct 2010
3. Review workshop team. Nov 2 - 5, 2010
4. Addition of Wounds and Abcesses Oct 2011 by Dr Hugh Cran
- For Infonet: Anne, Dr Hugh Cran
- For KARI: Dr Mario Younan KARI/KASAL, William Ayako - Animal scientist, KARI Naivasha
- For DVS: Dr Josphat Muema - Dvo Isiolo, Dr Charity Nguyo - Kabete Extension Division, Mr Patrick Muthui - Senior Livestock Health Assistant Isiolo, Ms Emmah Njeri Njoroge - Senior Livestock Health Assistant Machakos
- Pastoralists: Dr Ezra Saitoti Kotonto - Private practitioner, Abdi Gollo H.O.D. Segera Ranch
- Farmers: Benson Chege Kuria and Francis Maina Gilgil and John Mutisya Machakos
- Language and format: Carol Gachiengo
Information Source Links
- Barber, J., Wood, D.J. (1976) Livestock management for East Africa: Edwar Arnold (Publishers) Ltd 25 Hill Street London WIX 8LL. ISBN: 071310063X
- Bayer Leverkusen: Handbook for Farmers Stock Diseases. Germany Veterinary Dept
- Blood, D.C., Radostits, O.M. and Henderson, J.A. (1983) Veterinary Medicine - A textbook of the Diseases of Cattle, Sheep, Goats and Horses. Sixth Edition - Bailliere Tindall London. ISBN: 0702012866
- Blowey, R.W. (1986). A Veterinary book for dairy farmers: Farming press limited Wharfedale road, Ipswich, Suffolk IPI 4LG
- Force, B. (1999). Where there is no Vet. CTA, Wageningen, The Netherlands. ISBN 978-0333-58899-4.
- Hadrill David 2002: Horse Healthcare A Manual for Animal Health Workers and Owners ITDG Publishing ISBN 1 85339 486 6
- Hall, H.T.B. (1985). Diseases and parasites of Livestock in the tropics. Second Edition. Longman Group UK. ISBN 0582775140
- Hunter, A. (1996). Animal health: General principles. Volume 1 (Tropical Agriculturalist) - Macmillan Education Press. ISBN: 0333612027
- Hunter, A. (1996). Animal health: Specific Diseases. Volume 2 (Tropical Agriculturalist) - Macmillan Education Press. ISBN:0-333-57360-9
- ITDG and IIRR (1996). Ethnoveterinary medicine in Kenya: A field manual of traditional animal health care practices. Intermediate Technology Development Group and International Institute of Rural Reconstruction, Nairobi, Kenya. ISBN 9966-9606-2-7.
- M.M.H. Sewell and D.W. Brocklesby (Editors). Handbook on Animal Diseases in the Tropics, 4th ed. Balliere Tindall, London.
- Mackenzie & Simpson 1967: The African Veterinary Handbook Pitman Nairobi
- Merck Veterinary Manual 9th Edition
- Pagot, J. (1992). Animal Production in the Tropics and Subtropics. MacMillan Education Limited London. ISBN 0-333-53818-8
- The Organic Farmer magazine No. 50 July 2009

 Back
Back