|
Reproductive problems
|
| Introduction | Q Fever | |||
| Retained Placenta | Silent Heat | |||
| Anoestrus | Trichomoniasis | |||
| Brucellosis | Vibriosis | |||
| Endometritis | White Heifer Disease | |||
| Epivag | Review Process | |||
| Freemartinism | Information Source Links | |||
| Pyometra |
Introduction
Following the infectious disease, animals may end up with other related conditions such as Endrometitis and Pyometra.
All these result in lost income to the farmer as the animals may be unable to give birth again. Brucellosis and Q-fever are also highly contagious, and may transfer to people causing agonizing pain and sickness and very expensive medication, so paying close attention to the reproductive health of your animals is highly recommended.
Non-infectious conditions and other abnormalities include:
- Anoestrus
- Silent heat
- Freemartinism
- White heifer disease
When a herd of cows or sheep tend to have reduced number of calves, longer time before the female becomes pregnant, as well as when frequent abortions are observered or suspected, it is likely that a genital disease could be the problem. Farmers would in such cases be advised to invite a veterinarian to investigate the herd and take samples for analysis that can determine the cause of the problem. Reduced fertility in a herd means less profit and slower build up of herds.
Genital infections are spread through sexual contact between male and female animals. Unsually infected males do not show signs, but they can spread the disease to the female.
Retained Placenta
After giving birth cows sometimes do not drop the afterbirth (placenta) immediately. This can cause problems as decaying placenta tissue can cause a serious bacterial infection of the cow and if untreated the cow can even die.
Retention of afterbirth is usually defined as failure to expel the foetal membranes within 24 hours of giving birth.
Normally expulsion takes place within 3-8 hours after delivery of the calf.
The incidence of retained placenta in healthy dairy cows is 5 - 15%, while the incidence in beef cows is lower.
The incidence of retained placenta in healthy dairy cows is 5 - 15%, while the incidence in beef cows is lower.
Causes
The incidence is increased by abortion, difficult calvings, milk fever, twin births, advancing age of the cow, premature birth, inflammation of the placenta and various nutritional disturbances. With regard to the latter it should be noted that deficiencies of selenium, Vitamin A, copper and iodine increase the incidence of retained placenta. (Link to Nutritional deficiencies pls) Providing selenium prior to calving reduces the incidence of retained placenta.
There is a genetic implication and cows which retain their placenta in the presence of a nutritionally balanced diet should be considered for culling.
The incidence is higher in overweight cows.
The initiation of calving is a complex sequence of precisely timed endocrinal events and anything which disrupts this timing, such as premature calving, abortion, infection etc, will result in failure of the uterine muscle to function normally and failure to expel the afterbirth.
The precise mechanism of retained placenta (afterbirth) is not well understood. In a normal calving, degeneration and loosening of the placenta begins during late pregnancy. During calving changes in uterine pressure, reduction in blood flow and physical flattening of the uterine caruncles during uterine contractions lead to final loosening and expulsion of the foetal membranes.
Cows which fail to drop the afterbirth within 36 hours are likely to retain it for 7 -10 days. This is because substantial uterine contractions do not proceed beyond 36 hours of the birth of the calf and if the membranes have not been expelled by this time their subsequent separation from the uterine wall can only occur as a result of the rotting of the afterbirth connections to the uterus and their expulsion then depends on the speed of the normal shrinking of the uterus.
Diagnosis
This is normally straightforward. Degenerating, discoloured and increasingly unpleasant-smelling membranes are seen hanging from the vulva more than 24 hours after calving. Occasionally the retained membranes may remain within the uterus and may not be readily apparent, but their presence is usually signaled by a foul-smelling discharge.
Milk from cows with retained placenta must not be used for human consumption.
Usually there is no systemic illness. When there is, it is it is related to toxaemia (blood poisoning). Symptoms may include fever, lack of appetite, depression, a reduction in milk yield, straining, a foul smelling vaginal discharge and diarrhoea. These symptoms are more likely to occur in cases where retention follows extensive interference as in a difficult calving.
Usually there is no systemic illness. When there is, it is it is related to toxaemia (blood poisoning). Symptoms may include fever, lack of appetite, depression, a reduction in milk yield, straining, a foul smelling vaginal discharge and diarrhoea. These symptoms are more likely to occur in cases where retention follows extensive interference as in a difficult calving.
Treatment
Generally speaking uncomplicated cases of retained placenta require no treatment.
Manual removal of retained foetal membranes in the cow is NOT recommended and is potentially harmful.
Ideally stimulating uterine contractions by the use of drugs such as oxytocin or prostaglandins to expel the retained placenta is the most rational treatment. But after 24 hours there is very litttle response from the uterine muscle and so response to such treatment is unpredictable and generally poor.
In any event it is important not to adopt an inflexible approach to treatment. Trimming excess tissue which is objectionable to animal handlers and which contributes to gross contamination of the genital tract is permissible.
Should manual removal be decided upon one may attempt to remove the placenta if favourable circumstances are present: one should not resolve to remove the afterbirth at a particular time on every occasion.
No overdue force should be used and all due attention to strict hygiene must be paid.
Should there be systemic signs of illness, an examination by a veterinarian should be carried out to determine the cause and if necessary treatment with antibiotics and non steroidal anti-inflammatory drugs begun.
The insertion of pessaries into the uterus is NOT recommended. Generally the hand and arm which inserts the pessary is unsterile and placing a pessary adjacent to a putrefying placenta lacking a blood supply is valueless. Furthermore, if the pessary has any effect at all, it is to delay the rotting process and by so doing, prolong retention.
When an unusually high incidence of afterbirth retention is occurring in a herd then investigation to determine the common cause should be instituted.
All retention cases, irrespective of the method of treatment, or no treatment, should be examined by the vet at about 30 days after calving, and any showing signs of uterine infection treated by uterine infusion of antibiotic.
Sheep and goats may also be affected by retention of the placenta. Systemic treatment with antibiotics to guard against infection and gentle traction may be used.
Anoestrus
Diagnosis
Rectal examination by qualified vet to determine the cause.
Prevention
- Proper feeding and mineral supplementation of dairy cows including:
- Adequate quantity and good quality roughage.
- Adlibitum mineral supplementation.
Treatment
Treat the underlying cause. See Endometritis below.
Brucellosis
| Local Names: | Embua: kuyuna / Luo: tuo bwogo / Kikuyu: muhono, kihuna / Maasai: Aibiriu, olik, ibiroto / Samburu: ikiboroto /Swahili: homa ya kutupa mamba / Turkana: akiyech / Maragoli: Iuhusidza / Luyugusu: livure / Nandi: sutonik |
| Common Names: | Contageous abortion, Bang's disease |
| Scientific name: | Brucella abortus, Brucella melitensis, Brucella canis, Brucella suis |
| Description: | Reproductive problem and Zoonotic disease |
Introduction
Brucellosis is a bacterial infection, caused by organisms belonging to the genus Brucella. The disease is prevalent in most countries of the world. It primarily affects cattle, buffalo, pigs, sheep, goats, camels and dogs, and occasionally horses.
The disease in humans, sometimes called Undulant Fever, is a serious public health problem, especially when caused by Brucella Melitensis.
Brucellosis in cattle is caused almost exclusively by Brucella abortus, although occasionally Brucella melitensis or Brucella suis may be implicated. Melitensis occurs primarily in sheep and goats, suis in pigs, Brucella canis is confined to dogs.
Cattle of all ages and sex can be infected with B.abortus, but it is primarily a disease of sexually mature femal cattle, with bulls and immature animals showing little or no clinical disease.
Mode of Spread
- Natural transmission occurs by ingesting the bacteria, which are present in large numbers in aborted foetuses, foetal membranes and uterine discharges. Cattle may ingest contaminated feed or water, or lick contaminated genitals of other animals.
- Venereal transmission by infected bulls to susceptible cows appears to be rare, Brucella may enter the body through mucous membranes, the conjunctiva, wounds or intact skin.
- The disease is spread when aborting animals discharge B. abortus bacteria in the placenta, foetus and vaginal discharges to the ground, where they can survive for several weeks. Excertion of the bacteria may occur several days before abortion and for some time after. Cattle become infected when they ingest or inhale contaminated material.
- A cow's tail, heavily contaminated with infected ulterine discharges, may spread infection if it comes in contact with the conjunctiva or intact skin of other animals. The placenta, placental fluids, and foetus from an aborting animal contain organisms which contaminate the vulva, tail and legs of the animal and the surrounding environment.
- In in-calf females, the bacteria invade and cause abortion in the 7th month. The incubation period is about 6 weeks. It is only when a placenta exists i.e. in the second half of pregnancy, that the uterus is invaded and abortion occurs.
- Shedding from the vagina largely disappears with the decrease in fluids following calving. Some cows that previously aborted shed Brucella from the uterus following normal calvings.
- The disease can be transmitted to the unborn calf through the placenta by the infected dam. This disease can have serious negative economic consequences to stockmen in both modern intensive dairy systems and pastoral production enterprises.
- Organisms are shed in the milk for a variable period of time in most previously infected cattle for life.
- Housing or confining cattle increases the likelihood of transmission. Under range conditions the disease is of lower prevalence.
Spread to Man
- Man becomes infected when in direct contact with cows at abortion, calving or in the post calving period.
- Vets and stockhandlers are particularly at risk from the splashing of infected droplets into the eye.
- Infection occurs in people drinking unpasteurised milk or milk products.
- Symptoms include recurrent bouts of fever, headache, muscle and joint pains and general weakness. Brucellosis is often confused with malaria and influenza.
Signs of Brucellosis
- Abortion is the most obvious manifestation. Animals abort from the 7th month onwards.
- Infections may also cause still births or weak calves, retained placentas, and reduced milk yield. Usually general health is not affected in uncomplicated abortions.
- In less accute infections, cattle may give birth to a full term but weak calf, or merely show a retained placenta. Cows may become infertile due to chronic uterine infection.
- After abortion, the afterbirth doesn't come out (retained placenta). This can further develop to metritis (infection of the uterus), which often causes infertility.
- In bulls, no symptoms may be seen but if they are, they may include inflammation of the testes, lack of sexual activity and possibly infertility.
- Subcutaneous swellings containing infected fluid may appear on the legs of infected cattle and the placenta often has a thickened leathery appearance with necrosis of the cotyledons.
- Calves infected before puberty usually lose the infection once removed from the source of contamination.
- Mature non-pregnant animals, or animals in early pregnancy, when exposed to infection, are more likely to develop immunity than to show overt symptoms of disease.
Diagnosis This is based on the history, serology and bacteriology. Abortions occurring after 6 months of pregnancy are suggestive. However, blood samples should be taken for detailed laboratory analysis to confirm the disease.
- Serum samples should be taken for agglutination testing.
- When abortion occurs, aborted foetuses should be taken intact in a sealed container to the laboratory for detailed examinations. The organisms can be found in the placenta but more conveniently in pure culture in the stomach and lungs of an aborted foetus. All foetuses should be handled carefully with gloves to avoid human infection.
Diseases with Similar Symptoms
Abortion: See Vibriosis, Leptospirosis, Rift Valley Fever.
Prevention - Control - Treatment
Prevention and Control
- The disease can be controlled through effective sanitary measures in the cattle environment. Pregnant animals must be closely observed and any which show signs of aborting must be immediately isolated.
- Any animal which has aborted must be kept isolated until all uterine discharges have stopped. If there is any suspicion of infection, any animal about to calve should also be isolated.
- Under cool conditions the organism may survive for up to 2 months. Exposure to direct sunlight kills the organisms within a few hours.
- The use of plastic gloves and thorough disinfection of the vulva and tail of the cattle helps greatly to reduce the risk of infection when examining pregnant animals.
- Pasteurisation of milk and milk products renders them safe.
- Because of the danger of human infection, infected foetuses, placenta and cows should be handled with great care. Proper hygienic precautions should be taken when handling abortions and where infection is known to occur in certain herds of cattle. Handlers of such material should always wear gloves for protection. They should also ensure that they keep their hands away from the mouth, nose and eyes until after the hands are thoroughly disinfected.
- Burn and bury all contaminated materials such as foetuses and foetal membranes.
- Clean and disinfect all cattle premises which may be contaminated with foetuses and foetal membranes.
- Drinking of raw milk and unpasteurized milk products is dangerous.
Vaccination
- Calves between three and eight months should be vaccinated with live vaccine (S.19) to prevent infection. Such vaccinations can provide lifelong immunity against all but the heaviest challenge.
- The live vaccine should be used with care in adult animals because it can cause abortion in in-calf females and inflammation of the testes in adult males. It also results in persistent antibody titres if used in adults, making differentiation between atibody levels due to natural infection and vaccination very difficult. Adult cattle should therefore be vaccinated annually with dead B. abortus vaccine (45/20), or with a reduced dose - one twentieth - of S19 vaccine.
- S19 vaccine should be handled with care. It is a live vaccine and can infect humans.
- Vaccination will reduce the number of infected animals in a herd by over 90% if carried out over a period of 5 years. Vaccination cannot eradicate Brucellosis but it can lay the groundwork for future eradication.
- Bulls should not be vaccinated as the vaccine may result in the organism appearing in teh semen.
Recommended Treatment
Brucella infections are known to be persistent, so treatment with antibiotic is not recommended. It is therefore not practical and not useful to make any treatment attempt.
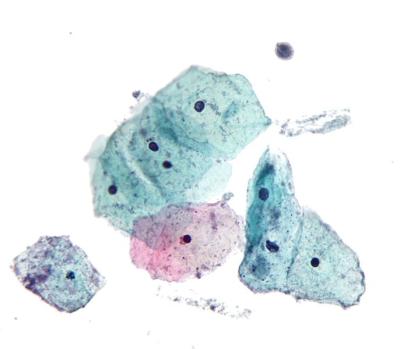
Endometritis
Clinical Signs
- Discharges.
- Repeated heat after mating.
Diagnosis
- History of repeated heat.
- Difficult calving.
- Retained placenta.
Prevention and Control
- Routine and strict hygiene at calving:
- Cows should be kept clean at calving.
- Ensure that calving boxes are cleaned and disinfected.
Treatment
Treat the underlying cause.
Epivag
|
Epivag is a rare chronic venereal infection of cattle probably caused by a virus. It occurs in East and Southern Africa. In the 1930s the disease was rampant in Eastern and Southern Africa, prompting the creation of the world's first national AI service to control it in Kenya. It has now become sporadic and reports are unusual.
The infection is spread by coitus or contaminated obstetrical equipment.
Signs of Epivag
Epivag is characterized by enlargement and induration of the epididymis in the bull and vaginitis, cervicitis and endometritis in the cow.
Only cattle are affected. Indigenous African cattle possess a high natural resistance and signs of Epivag in them are rare. Imported exotic cattle and their crosses have little resistance.
Affected bulls have enlarged and distorted testes. The lesions take 3-6 months to develop and sometimes longer. Enlargement of the head and tail of the epididymis occurs. Often both epididymses are affected. Bulls are at first infertile and then sterile. The semen is affected before clinical signs are apparent. The volume is reduced, the appearance is watery and floccules of mucus appear.
The incubation period in cows lasts only a few days but the infection persists for months. In cows, the clinical signs vary from slight reddening of the vagina with little or no discharge to severe inflammation of the inner lining of the vagina, cervix and uterus with profuse thick yellowish discharges. Infection usually persists for several months in cows with most of them recovering while a few may become permanently sterile.
Diagnosis
Diagnosis is based on the herd history, the clinical signs, and the semen examiniation. Lesions in the female are difficult to assess in the absence of the disease in the male.
Diseases with Similar Symptoms
The clinical signs in the female are easily confused with those of Infectious Pustular Vulvovaginitis. Lesions in Epivag, however, persist for many weeks.
Prevention and Control
Use of artificial insemination with semen from clean bulls is an effective control measure. All affected bulls should be slaughtered.
Recommended treatment
Because the specific cause is uncertain, no attempt should be made to treat the bulls, but cows can be treated symptomatically by a veterinarian and then later inseminated.
The widespread use of artificial insemination using semen from clean bulls has brought the disease under control dramatically in Eastern and Southern Africa.
Freemartinism
Diagnosis
- History of twin male and female calves.
- Failure of estrus to occur.
Prevention and Control
Culling of freemartin heifers.
Treatment
None.
Pyometra
Clinical Signs
- Enlarged uterus.
- Discharge of pus when the cow lies down.
Diagnosis
- Uterus palpataion by a veterinarian.
- Uterus scan.
Recommended Treatment
Treatment used by estrogens and oxytocin.
Q Fever
Introduction
Q Fever was first identified in Queensland, Australia; hence its name.
This is a bacterial disease and an important zoonosis (an animal disease that can be transmitted to humans). Q Fever is caused by an organism called Coxiella burnetii. It is found all over the world, in every country where it has been sought.
Its main importance is its ability to infect man, and to cause abortions, metritis (inflammation of the lining of the uterus), and mastitis in infected ruminants.
Coxiella burnetii is an extremely difficult organism to eliminate. It is very tough, resisting most disinfectants, heat and drying, and surviving for years in dust.
Mode of Spread
There are two different cycles:
1. The bacterium cycles between small free-living ground mammals and ticks.
2. The bacterium cycles in domestic ruminants (cattle, sheep, goats), independent of the wild animal cycle.
Ticks can act as reservoirs of the organism. Tick-free cycles in domestic ruminants allow the organism to be concentrated in the genital tract and udder, from where large numbers are shed in milk, faeces or urine, or, from the genital tract at lambing or calving.
A wide variety of other animals and birds may also be affected and play a part in spreading Coxiella burnetti. These include dogs and several species of birds.
At-risk animals, and man, become infected by inhaling infected fluid discharges in the air or dust loaded with dried discharges.
The disease is highly infectious. Animal handlers are particularly at risk from infection, especially at lambing or calving, from inhalation, ingestion or direct contact with birth fluids or afterbirth.
However the main route of most human infections is by inhalation of contaminated air droplets or dust originating in infected ruminants or other animals e.g. cats.
Spread can occur up to 10 kilometers from the source of infection by wind dispersal of dried reproductive products, such as afterbirth, genital discharges, etc from infected sheep, cattle and goats, depending on wind condition.
Symptoms of Q Fever
- Infection in ruminants is usually symptom-free, but it can cause late abortions, inflammation of the uterus and mastitis in sheep and goats, together with loss of appetite, and offspring of carrier animals can often appear weak, showing low vitality. Large numbers of organisms are shed in the milk, urine, faeces, saliva and especially through the afterbirth and uterine discharges. These are the main sources of infection for man.
Cows may shed the organism in milk for years. - Symptoms of Q Fever in man can easily be mistaken for those of flu: fever, headache, chills, muscle pains, lack of appetite and nausea. The incubation period is about 2 to 3 weeks, and the disease lasts for 1-2 weeks.
- In severe and chronic cases, pneumonia, hepatitis and endocarditis may occur and in some cases the infection causes death, as has happened in the recent outbreak in north-west Europe.
- The infection of pregnant women can result in abortion or premature delivery.
- The main route of infection is by inhalation of infected dust or aerosol droplets. Drinking contaminated raw milk products is unlikely to cause any symptoms of disease.
Diagnosis
There are no clinical signs in domesticated animals. The sudden appearance of an influenza-like disease in man following an association with cattle, sheep or goats, or with their carcases, hides, tissues, or following an autopsy, should be regarded as evidence of infection.
But neither the history nor the clinical picture is enough to prove the presence of Q Fever. A definite diagnosis can be established only by lab tests to identify the bacteria that causes the disease in teh blood or sputum of a patient.
Other causes of abortion in ruminants should be considered when reaching a diagnosis.
Prevention - Control - Treatment
Control
Recovered animals remain infected and infective for many years and sometimes for life. It is therefore necessary to take the steps to limited the spread of infection by adopting hygienic precautions at the time of lambing, kidding and calving. In particular afterbirths should be destroyed. In known infected flocks or herds pregnant animals should be separated from others indoors.
Vaccines are available and are being developed in Europe and when giving to uninfected animals have prevented infection. When given to previously infected animals the vaccines have improved fertility and reduced the shedding of organisms.
This disease is probably much more common than is realized, due to under reporting and lack of facilities in reaching a diagnosis.
Treatment
In animals this is seldom attempted. Oral tetracyclines are reported to have a beneficial effect, but their use carries risks in ruminating animals such as cows, and is therefore not recommended.
Silent Heat
Clinical Signs
- Small vulva.
- Long tuft of hair at the ventral end of the vulva.
- Clitoris is prominent when you open the vulva.
- Complete anoestrus.
Diagnosis
Rectal palpation and use of breeding records.
Prevention
- Proper feeding and mineral supplementation of dairy cows including:
- Adequate quantity and good quality roughage.
- Adlibitum mineral supplementation.
- Timely and regular heat detection.
Treatment
Use of hormones.
Trichomoniasis
Mode of Spread
The infection is spread by coitus or through the use of contaminated insemination instruments or stockmen's hands.
T.foetus infection is confined to the reproductive tract where it can invade most parts. Infection normally lasts about 3 months. There is usually a mild inflammation of the vagina shortly after infection but significant changes do not normally take place until 50-60 days after infection when vaginitis, cervicitis, endometritis, pyometra and early abortion may take place.
Abortions are often undetected and the main feature observed is often a failure of cows to hold to service.
Infection in the male is usually confined to the surface of the prepuce and penis and is usually so mild it is not clinically apparent.
Signs of Trichomoniasis
- Cows may have a profuse watery vaginal discharge about 2 weeks after coital infection.
- Abortion may occur in early or late in pregnancy.
- There is irregular oestrus which may cease altogether.
- Cows eventually clear themselves of infection and the uterus is usually normal 2-6 months after infection.
- Bulls show no symptoms but once infected tend to remain permanent carriers.
Diagnosis
Trichomoniasis can be suspected in any breeding cattle if there is a history of reproductive failure characterized by repeated returns to service a lower than expected pregnancy rate a wide range of gestational ages and cases of early abortion and pyometra.
Laboratory diagnosis is possible and can be made from a foetus, placental fluids, uterine contents, or via mucus taken from the vagina or from the prepuce of a bull.
Diseases with Similar Symptoms
The disease must be differentiated from Vibriosis which it resembles.
Prevention and Control
- The simplest control method involves ceasing to breed cows for at least 3 months, by which time they will have eliminated the infection, and to carry out examination of the cervical mucus using the vaginal mucus agglutination.
- Use of a clean bull either for natural mating or artificial insemination is also a control method.
Recommended treatment
The majority of infected cows and heifers recover completely and clear the infection and so they are not normally treated.
In bulls treatment using various imidazoles has been used but none is both safe and effective. Ipronidazole is probably the most effective but can cause sterile abscesses at the injection site. In addition bulls are probably susceptible to re-infection after successful treatment.
Resistance to iponidazole may be a concern. The biggest problem, however, is that the success of treatment is measured by repeat sampling which may mean that the individual bull can never be definitely said to be negative. Therefore it is better to cull bulls and replace them with virgin bulls or to test and cull positive bulls.
Re-infection is prevented by exposing only uninfected (clean) bulls to uninfected (clean) cows. Clean cows are assumed to be those with calves at foot and virgin heifers.
Vibriosis
| Scientific Name: | Campylobacter fetus venerealis and Campylobacter fetus fetus |
| Common Names: | Bovine campylobacteriosis, Genital vibriosis |
Vibriosis is a bacterial venereal disease of cattle and sheep characterized primarily by early embryonic death, infertility, a protracted calving season and occasionally by abortion. It occurs worldwide.
It is caused by bacteria called Campylobacter fetus, Venerealis and Campylobacter fetus fetus. C. fetus fetus was thought for many years to be primarily an intestinal organism but it has been found to be a significant cause of the classic infertility syndrome usually attributed to C. fetus venerealis.
Vibriosis in sheep is evidenced by abortions in late pregnancy and still births.
Mode of Spread
In cattle the disease is transmitted venereally by coitus. It is also trasmitted by contaminated instruments, bedding or by artificial insemination using contaminated semen. Individual bulls vary in their susceptibility to infection. Some become permanent carriers, while others appear to be resistent to infection. In young bulls, less than 3-4 years of age, infection tends to be temporary with transmission apparently relying on sexual contact with a non-infected cow within minutes to days of breeding with an infected cow. Spontaneous clearance in these younger bulls does not seem to be related to any immunte response and so re-infection can readily occur. Bulls older than 3-4 years are more likely to suffer chronic infections.
Some cows clear the infection rapidly, others carry it for up to or longer than 2 years. Although most of the genital tract may be free of infection, when a cow eventually conceives the vagina may remain chronically infected throughout pregnancy.
Some infected females can maintain pregnancy but abort usually around the fifth month of pregnancy or sometimes earlier. This means that the presence of the disease can go un-noticed without proper herd fertility records. Breeding females eventually eliminate the infection six months after being infected at service and recover completely. They are then immune and can breed normally.
Signs of Vibriosis
Vibriosis affects both breeding males and females but clinical signs of temporary infertility are confirmed to females. Clincal signs, other than reproductive failure or abortion, are minimal or absent. The infection of females at conception results in infection in teh anterior vagina which subsequently spread to teh uterus and fallopian tubes. The infection persists for months and causes the developing foetus to die. The embryonic death initiates cyclical activity in the ovary but these cycles are often irregular with prolonged intervals. Observed abortions are uncommon.
Clinical signs in herds for which good records are maintained are soon evident shortly after the introduction of an infected bull. Animals which have been presumed to have been in calf have irregular returns to heat. In more extensive systems using natural service infection may not be suspected until the calving pattern indicates a delay in conception and a reduced calf crop.
Where the disease has been present for some time indications that C. fetus is present may be much less dramatic, with only heifers, calved heifers and a few susceptible cows being affected, as older animals have acquired natural immunity.
Bulls show no symptoms and produce normal semen. In other words they are fertile, generally virile, and provided they do not have to serve too many returning females, active. The females they server conceive, but they have been infected. Subsequently the foetus dies and they return to service.
The disease in sheep manifests with abortions in late pregnancy and still births. Ewes may develop metritis (inflammation of the uterus) after expelling the foetus, which is usually rotten, with 40% having orange-yellow spots in the liver. The disease in sheep is acquired by mouth, not via the ram.
Diagnosis
This would be based on the history of late abortions and return to heat after successful mating.
Laboratory diagnosis is based on the vaginal mucus agglutination test. Samples are taken from at least 10% of the herd, concentrating on those females most recently exposed to infection by service, open cows or those returning to their third or fourth service. Tampons are placed in the anterior vagina and sheath washings are taken from suspected bulls.
Prevention and Control
- Use of Artificial insemination with semen from non-infected bulls should eliminate the infection from an infected herd by the end of two pregnancies.
- Care must be taken when buying breeding bulls. A veterinary certificate stating that they are free of Vibriosis (and Trichomoniasis) should be insisted upon.
- Where AI is not feasible, all animals in a herd should be tested and the infected and non-infected animals managed separately. This approach requires a high level of management and careful veterinary supervision.
- Vaccination is practiced where the vaccine is available
- In sheep strict hygiene and regular vaccination, where the vaccine is available, should be practiced.
Recommended treatment
Treatment in breeding females is rarely effective or practical since the organism is eliminated. Males remain infected permanently and therefore necessary to clear them of the organism. The infection can be eliminated in bulls through treatment with antibiotics by a qualified vet. One or two treatments with 20mg/kg of Streptomycin, together with 5g of Streptomycin in an oil based suspension applied to the penis and the lining of the prepuce for 3 consecutive days is effective. Bulls are of course susceptible to re-infection if they mate with an infected female.
In sheep the use of tetracyclines may help to prevent exposed ewes from aborting.
White Heifer Disease
Review Process
2. Hugh Cran, Practicing Veterinarian Nakuru. March - Oct 2010.
3. Review workshop team. Nov 2 - 5, 2010.
- For Infonet: Anne, Dr Hugh Cran
- For KARI: Dr Mario Younan KARI/KASAL, William Ayako - Animal scientist, KARI Naivasha
- For DVS: Dr Josphat Muema - Dvo Isiolo, Dr Charity Nguyo - Kabete Extention Division, Mr Patrick Muthui - Senior Livestock Health Assistant Isiolo, Ms Emmah Njeri Njoroge - Senior Livestock Health Assistant Machakos
- Pastoralists: Dr Ezra Saitoti Kotonto - Private practioner, Abdi Gollo H.O.D. Segera Ranch
- Farmers: Benson Chege Kuria and Francis Maina Gilgil and John Mutisya Machakos
- Language and format: Carol Gachiengo
Information Source Links
- Barber, J., Wood, D.J. (1976) Livestock management for East Africa: Edwar Arnold (Publishers) Ltd 25 Hill Street London WIX 8LL. ISBN: 071310063X
- Blood DC, Henderson JA, Radostits OM (1983): Veterinary medicine: A textbook of the diseases of cattle, sheep, pigs & horses. 6th Edition. Bailliere and Tindall, 24-28 Oval Road, London NW1 7DX, UK. ISBN NO: 0-7020-0988-1.
- Force, B. (1999). Where there is no Vet. CTA. Wageningen. The Netherlands. ISBN 978-0333-58899-4.
- Handbook on Animal Diseases in the Tropics 4th Edition Sewell & Brocklesby
- Henning MW (1956): Animal Diseases in South Africa, 3rd Edition. Onderstepoort Veterinary Institute, Central News Agency Ltd., Pretoria, South Africa
- Hunter, A. (1996). Animal health: General principles. Volume 1 (Tropical Agriculturalist) - Macmillan Education Press. ISBN: 0333612027
- Khan CM and Line S (2005): The Merck Veterinary Manual, 9th Edition, Merk & Co Inc Whitehouse Station NJ USA. ISBN 0-7020-1502-4
- Merck Veterinary Manual 9th Edition 2005 ISBN Number : 0-911910-50-6
- Q Fever booklet, CEVA Sante Animal, France
- Veterinary Medicine A Textbook of the Diseases of Cattle, Sheep, Pigs, Goats and Horses Blood, Radostits & Henderson 6th Edition 1983 Bailiere Tindall 1 St Anne?s Road, Eastbourne England BN21 3UN ISBN 0 7020 0988 1
- Veterinary Reproduction and Obstetrics 5th Edition 1986 Arthur, Noakes & Pearson Bailliere Tindall 33 The Avenue Eastbourne, East Sussex, England BN21 3UN
- lowey, R.W. (1986). A Veterinary book for dairy farmers: Farming press limited Wharfedale road, Ipswich, Suffolk IPI 4LG

 Back
Back