Radioisotopes in medicine
| Topics: |
This EOE article is adapted from an information paper published by the World Nuclear Association (WNA). WNA information papers are frequently updated, so for greater detail or more up to date numbers, please see the latest version on WNA website (link at end of article).
Contents
Radioisotopes
Many of the chemical elements have a number of isotopes. The isotopes of an element have the same number of protons in their atoms (atomic number) but different masses due to different numbers of neutrons. In an atom in the neutral state, the number of external electrons also equals the atomic number. These electrons determine the chemistry of the atom. The atomic mass is the sum of the protons and neutrons. There are 82 stable elements and about 275 stable isotopes of these elements.
When a combination of neutrons and protons that does not already exist in nature is produced artificially, the atom will be unstable and is called a radioactive isotope or radioisotope. There are also a number of unstable natural isotopes arising from the decay of primordial uranium and thorium. Overall there are some 1800 radioisotopes.
At present, there are up to 200 radioisotopes used on a regular basis, and most must be produced artificially. Radioisotopes can be manufactured in several ways. The most common is by neutron activation in a nuclear reactor. This involves the capture of a neutron by the nucleus of an atom resulting in an excess of neutrons (neutron rich). Some radioisotopes are manufactured in a cyclotron in which protons are introduced to the nucleus resulting in a deficiency of neutrons (proton rich).
The nucleus of a radioisotope usually becomes stable by emitting an alpha and/or beta particle (or positron). These particles may be accompanied by the emission of energy in the form of electromagnetic radiation known as gamma rays. This process is known as radioactive decay.
Radioactive products that are used in medicine are referred to as radiopharmaceuticals.
Nuclear Medicine
Nuclear medicine is a branch of medicine that uses radiation to provide information about the functioning of a person's specific organs or to treat disease. In most cases, the information is used by physicians to make a quick, accurate diagnosis of the patient's illness. The thyroid, bones, heart, liver and many other organs can be easily imaged, and disorders in their function revealed. In some cases, radiation can be used to treat diseased organs, or tumors. Five Nobel Laureates have been intimately involved with the use of radioactive tracers in medicine.
Over 10,000 hospitals worldwide use radioisotopes in medicine, and about 90% of the procedures are for diagnosis. The most common radioisotope used in diagnosis is technetium-99, with over 30 million procedures per year.
In developed countries (26% of world population) the frequency of diagnostic nuclear medicine is 1.9% per year, and the frequency of therapy with radioisotopes is about one-tenth of this. The use of radiopharmaceuticals in diagnosis is growing at over 10% per year.
Nuclear medicine was developed in the 1950s by physicians with an endocrine emphasis, initially using iodine-131 to diagnose and then treat thyroid disease. In recent years, specialists have also come from radiology, as dual CT/PET procedures have become established.
Diagnosis
Diagnostic techniques in nuclear medicine use radioactive tracers that emit gamma rays from within the body. These tracers are generally short-lived isotopes linked to chemical compounds that permit specific physiological processes to be scrutinized. They can be given by injection, inhalation or orally. The first type are where single photons are detected by a gamma camera that can view organs from many different angles. The camera builds up an image from the points from which radiation is emitted; this image is enhanced by a computer and viewed by a physician on a monitor for indications of abnormal conditions.
A more recent development is Positron Emission Tomography (PET), a more precise and sophisticated technique using isotopes produced in a cyclotron. A positron-emitting radionuclide is introduced, usually by injection, and accumulates in the target tissue. As it decays, it emits a positron, which promptly combines with a nearby electron resulting in the simultaneous emission of two identifiable gamma rays in opposite directions. These are detected by a PET camera and give very precise indication of their origin. PET's most important clinical role is in oncology (the branch of medicine concerned with the study and treatment of tumors), with fluorine-18 as the tracer, since it has proven to be the most accurate non-invasive method of detecting and evaluating most cancers. It is also well used in cardiac and brain imaging.
New procedures combine PET with CT scans to give co-registration of the two images, enabling 30% better diagnosis than with a traditional gamma camera alone. It is a very powerful and significant tool which provides unique information on a wide variety of diseases from dementia to cardiovascular disease and cancer (oncology).
Positioning of the radiation source within the body makes the fundamental difference between nuclear medicine imaging and other imaging techniques such as x-rays. Gamma imaging by either method described provides a view of the position and concentration of the radioisotope within the body. Organ malfunction can be indicated if the isotope is either partially taken up in the organ (cold spot), or taken up in excess (hot spot). If a series of images is taken over a period of time, an unusual pattern or rate of isotope movement could indicate malfunction in the organ.
A distinct advantage of nuclear imaging over x-ray techniques is that both bone and soft tissue can be imaged very successfully. This has led to its common use in developed countries where the probability of anyone having such a test is about one in two and rising.
The mean effective radiation dose is 4.6 mSv per diagnostic procedure.
Radiotherapy
Rapidly dividing cells are particularly sensitive to damage by radiation. For this reason, some cancerous growths can be controlled or eliminated by irradiating the area containing the growth. External irradiation can be carried out using a gamma beam from a radioactive cobalt-60 source, though in developed countries the much more versatile linear accelerators are now being utilized as a high-energy x-ray source (gamma and x-rays are much the same).
Internal radiotherapy is carried out by administering or planting a small radiation source, usually a gamma or beta emitter, in the target area. Iodine-131 is commonly used to treat thyroid cancer, probably the most successful kind of cancer treatment. It is also used to treat non-malignant thyroid disorders. Iridium-192 implants are used especially in the head and breast. They are produced in wire form and are introduced through a catheter to the target area. After administering the correct dose, the implant wire is removed to shielded storage. This brachytherapy (short-range) procedure gives less overall radiation to the body, is more localized to the target tumor and is cost-effective.
Treating leukaemia may involve a bone marrow transplant, in which case the defective bone marrow will first be killed off with a massive (and otherwise lethal) dose of radiation before being replaced with healthy bone marrow from a donor.
Many therapeutic procedures are palliative, usually to relieve pain. For instance, strontium-89 and, increasingly, samarium-153 are used for the relief of cancer-induced bone pain. Rhenium-186 is a newer product used in these treatments.
A new field is Targeted Alpha Therapy (TAT), especially used for the control of dispersed cancers. The short range of very energetic alpha emissions in tissue means that a large fraction of that radiative energy goes into the targeted cancer cells, once a carrier has taken the alpha-emitting radionuclide to exactly the right place. Laboratory studies are encouraging and clinical trials for leukaemia, cystic glioma and melanoma are underway.
An experimental development of this field is Boron Neutron Capture Therapy using boron-10 that concentrates in malignant brain tumors. The patient is then irradiated with thermal neutrons which are strongly absorbed by the boron, producing high-energy alpha particles that kill the cancer. This requires the patient to be brought to a nuclear reactor, rather than the radioisotopes being taken to the patient.
Radiotherapy has progressively become successful in treating persistent disease and doing so with low toxic side-effects. With any therapeutic procedure, the aim is to confine the radiation to well-defined target volumes of the patient. The [[dose]s] per therapeutic procedure are typically 20-60 Gy.
Biochemical analysis
It is very easy to detect the presence or absence of some radioactive materials even when they exist in very low concentrations. Radioisotopes can therefore be used to label molecules of biological samples in vitro (out of the body). Pathologists have devised hundreds of tests to determine the constituents of blood, serum, urine, hormones, antigens and many drugs by means of associated radioisotopes. These procedures are known as radioimmuno-assays and, although the biochemistry is complex, kits manufactured for laboratory use are very easy to use and give accurate results. In Europe some 15 million of these in vitro analyses are undertaken each year.
Diagnostic Radiopharmaceuticals
Every organ in our bodies acts differently from a chemical point of view. Doctors and chemists have identified a number of chemicals that are absorbed by specific organs. The thyroid, for example, takes up iodine, the brain consumes quantities of glucose, and so on. With this knowledge, radiopharmacists are able to attach various radioisotopes to biologically active substances. Once a radioactive form of one of these substances enters the body, it is incorporated into the normal biological processes and excreted in the usual ways.
Diagnostic radiopharmaceuticals can be used to examine blood flow to the brain, functioning of the liver, lungs, heart or kidneys, to assess bone growth, and to confirm other diagnostic procedures. Another important use is to predict the effects of surgery and assess changes since treatment.
The amount of the radiopharmaceutical given to a patient is just sufficient to obtain the required information before its decay. The radiation dose received is medically insignificant. The patient experiences no discomfort during the test and after a short time there is no trace that the test was ever done. The non-invasive nature of this technology, together with the ability to observe an organ functioning from outside the body, makes this technique a powerful diagnostic tool.
A radioisotope used for diagnosis must emit gamma rays of sufficient energy to escape from the body and it must have a half-life short enough for it to decay away soon after imaging is completed.
The radioisotope most widely used in medicine is technetium-99m, employed in some 80% of all nuclear medicine procedures—70,000 every day. It is an isotope of the artificially-produced element technetium and it has almost ideal characteristics for a nuclear medicine scan. These are:
- It has a half-life of six hours, which is long enough to examine metabolic processes yet short enough to minimize the radiation dose to the patient;
- Technetium-99m decays by a process called "isomeric"; which emits gamma rays and low-energy electrons. Since there is no high-energy beta emission, the radiation dose to the patient is low;
- The low energy gamma rays it emits easily escape the human body and are accurately detected by a gamma camera. Once again, the radiation dose to the patient is minimized; and
- The chemistry of technetium is so versatile it can form tracers by being incorporated into a range of biologically-active substances to ensure that it concentrates in the tissue or organ of interest.
Its logistics also favor its use. Technetium generators, a lead pot enclosing a glass tube containing the radioisotope, are supplied to hospitals from the nuclear reactor where the isotopes are made. They contain molybdenum-99, with a half-life of 66 hours, that progressively decays to technetium-99. The Tc-99 is washed out of the lead pot by saline solution when it is required. After two weeks or less, the generator is returned for recharging.
A similar generator system is used to produce rubidium-82 for PET imaging from strontium-82, with a half-life of 25 days.
Myocardial Perfusion Imaging (MPI) uses thallium-201, chloride, or technetium-99m and is important for detection and prognosis of coronary artery disease.
For PET imaging, the main radiopharmaceutical is Fluoro-deoxy glucose (FDG) incorporating F-18, with a half-life of just under two hours, as a tracer. The FDG is readily incorporated into the cell without being broken down, and is a good indicator of cell metabolism.
In diagnostic medicine, there is a strong trend for using more cyclotron-produced isotopes, such as F-18, as PET and CT/PET become more widely available. However, the procedure needs to be undertaken within two hours reach of a cyclotron.
Therapeutic Radiopharmaceutical
For some medical conditions, it is useful to destroy or weaken malfunctioning cells using radiation. The radioisotope that generates the radiation can be localized in the required organ in the same way it is used for diagnosis—through a radioactive element following its usual biological path, or through the element being attached to a suitable biological compound. In most cases, it is beta radiation that causes the destruction of the damaged cells; this is radiotherapy. Short-range radiotherapy is known as brachytherapy, and this is becoming the main means of treatment.
Although radiotherapy is less common than diagnostic use of radioactive material in medicine, it is nevertheless widespread, important and growing. An ideal therapeutic radioisotope is a strong beta emitter with just enough gamma to enable imaging, e.g., lutetium-177. This is prepared from ytterbium-176 that is irradiated to become Yb-177, which decays rapidly to Lu-177. Yttrium-90 is used for treatment of cancer, particularly non-Hodgkin's lymphoma, and its more widespread use is envisaged, including for arthritis treatment.
Iodine-131 and phosphorus-32 are also used for therapy. Iodine-131 is used to treat the thyroid for cancers and other abnormal conditions such as hyperthyroidism (over-active thyroid). In a disease called Polycythemia vera, an excess of red blood cells is produced in the bone marrow. Phosphorus-32 is used to control this excess.
A new and still experimental procedure uses boron-10, which concentrates in the tumor. The patient is then irradiated with neutrons which are strongly absorbed by the boron, to produce high-energy alpha particles that kill the cancer.
For targeted alpha therapy (TAT), actinium-225 is readily available now, from which the daughter Bi-213 can be obtained (via 3 alpha decays) to label targeting molecules.
Considerable medical research is being conducted worldwide into the use of radionuclides attached to highly specific biological chemicals such as immunoglobulin molecules (monoclonal antibodies). The eventual tagging of these cells with a therapeutic dose of radiation may lead to the regression—or even cure—of some diseases.
Radioisotope poison
In 2006 Britain witnessed the apparent murder of one of its newer citizens, a former Russian intelligence official, by poisoning with radioactive polonium. His death was slow and excruciating.??
Polonium has about 26 isotopes, all of which are radioactive. Webelements periodic table says that it is 250 billion times more toxic than hydrocyanic acid. It is readily soluble in weak acid. (It was the first element discovered by Marie Curie, in 1898, and named after her native Poland. Her daughter Irene was contaminated with polonium in a laboratory accident and died of leukemia at the age of 59.)
Polonium-210 is the penultimate decay product of U-238, before it alpha decays to become stable lead. It results from the beta decay of Pb-210 (in the U-238 decay series) to Bi-210 which rapidly beta decays to Po-210. This gives rise to its occurrence in nature, where uranium is ubiquitous. However, because of its short (138 day) half life, very little Po-210 would be found in uranium ore or mill tailings (Webelements suggests 0.1 mg/tonne).??Po-210 levels in soil would be even less, but it is concentrated in tobacco and traces of it can be found in smokers' urine.??
Po-210 can also be made by neutron irradiation of Bi-209, and that is most likely source of any significant quantity. Russia has used Po-210 as a heat source in short-life spacecraft and lunar rovers. It also operates reactors using lead-bismuth cooling, which becomes contaminated with Po-210 due to neutron bombardment.??
Because its half-life is so short, a gram of Po-210 is about 5000 times as radioactive as a gram of radium - which sets the standard of activity. But at 138 days its half life is long enough for it to be manufactured, transported and administered before its loses its potency. It would not put the carrier at much risk, since alpha radiation is only really a hazard inside the body - a layer of skin is protection. About 10 micrograms (2 GBq) was said to have been used, administered in a cup of tea (it would be warm due to the decay).
However, simply dosing someone with polonium might not have much effect if it simply went in one end and out the other in a day or two without being absorbed from the gut. It would probably need to be complexed on to an organic carrier which would enter the bloodstream and take it to vital organs where it would stay. (This is what happens with targeted alpha therapy (TAT) using very low levels of alpha-active radioisotopes: the carriers take them to dispersed cancerous tissues where they are needed.)?
In Mr Litvinenko's case the intense alpha radiation was reportedly in vital organs and sufficient to destroy them over three weeks. It was apparently over one hundred times the dose used in TAT for cancer treatment and the Po-210 is much longer-lived than isotopes used for TAT. It could have been attached to something as simple as a sugar.?
Supplies of radioisotopes
Medical radioisotopes made in nuclear reactors are sourced from relatively few reactors, including:
NRU at Chalk River in Canada (supplied via MDS Nordion)
HFR at Petten in Netherlands (supplied via IRE and Tyco)
BR2 at Mol in Belgium (supplied via IRE and Tyco)
Osiris & Orphee at Saclay in France (supplied via IRE)
FRJ-2/ FRM-2 at Julich in Germany (supplied via IRE)
LWR-15 at Rez in Czech Republic
HFETR at Chengdu in China
Safari in South Africa (supplied from NTP)
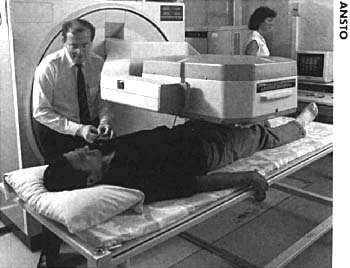
Opal in Australia (supplied from ANSTO).
Of fission radioisotopes, 40% of Mo-99 (for Tc-99m) comes from MDS Nordion, 25% from Tyco, 20% from IRE and 10% from NTP. For I-131, 75% is from IRE, 25% from NTP.
A number of incidents in 2008 pointed up shortcomings and unreliability in the supply of isotopes, particular technetium. Some 95% of the world's supply of this comes from only five reactors, all of them over 40 years old. Also the processing and distribution of isotopes is complex and constrained, which can be critical when the isotopes concerned are short-lived. A need for increased production capacity and more reliable distribution is evident.
Wastes
The use of radioisotopes for medical diagnosis and treatments results in the generation of mainly Low-Level Waste (LLW). This waste includes paper, rags, tools, clothing and filters, which contain small amounts of mostly short-lived radioactivity. These types of waste often undergo decay storage for periods of months to a few years before being disposed of at urban land-fill sites.
When radiography sources have decayed to a point where they are no longer emitting enough penetrating radiation for use in treatments, they are considered as radioactive waste. Sources such as Co-60 are treated as short-lived Intermediate-Level wastes (ILW). Other sources such as Radium-226, used in cancer therapy, will however require long-term storage and geological disposal as ILW, as a result of their higher level of long-lived radioactivity.
Further Reading
- WNA paper on Radioisotopes in medicine
- ANSTO, and papers at 1999 and 2001 ANA conferences.
- NRPB Bulletin #231, Sept 2001.