Ecosystems and Human Well-being: Health Synthesis: Summary for Decision-Makers
This is part of the Millenium Ecosystem Assessment report Ecosystems and Human Well-being: Health Synthesis.
Core Writing Team: Carlos Corvalan, Simon Hales, Anthony McMichael
Extended Writing Team: Colin Butler, Diarmid Campbell-Lendrum, Ulisses Confalonieri, Kerstin Leitner, Nancy Lewis, Jonathan Patz, Karen Polson, Joel Scheraga, Alistair Woodward, Maged Younes and many MA authors.
Review Editors: José Sarukhán and Anne Whyte (co-chairs); Philip Weinstein and other members of the MA Board of Review Editors.
| The health impacts of ecosystem change are global as well as local; here dust from north Africa is distributed widely across the continent, with potential impacts on health. Degradation of drylands, as well as biomass burning, exacerbates problems associated with dust storms. |
Contents
- 1 Why do ecosystems matter to human health?
- 2 Ecosystem services and human health
- 3 How have ecosystems changed and what are the health implications?
- 4 How might ecosystems change and what would be the health implications?
- 5 What actions would address the health consequences of ecosystem change?
- 6
- 7 ==
Why do ecosystems matter to human health?
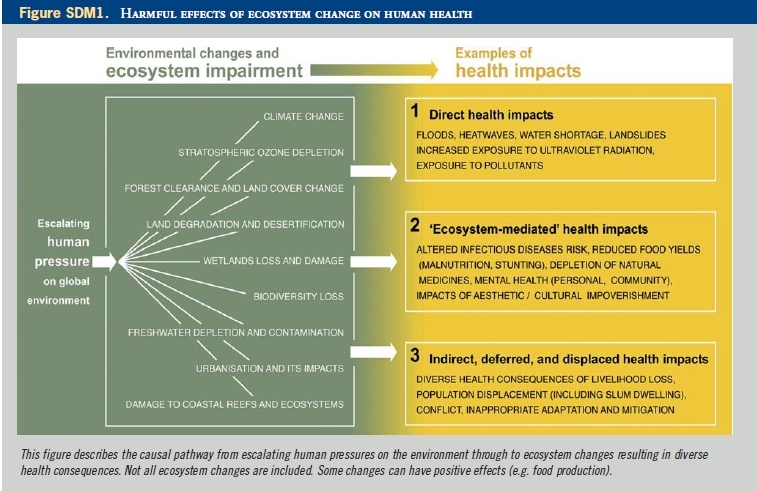
Ecosystems are the planet's life-support systems - for the human species and all other forms of life. Human biology has a fundamental need for food, water, clean air, shelter and relative climatic constancy. Other health benefits include those derived from having a full complement of species, intact watersheds, climate regulation and genetic diversity. Stresses on freshwater sources, food-producing systems and climate regulation could cause major adverse health impacts (high certainty) (see Figure SDM1).
Ecosystem services are indispensable to the well-being and health of people everywhere. In addition to providing life's basic (above-mentioned) needs, changes in their flow affect livelihoods, income, local migration and, on occasion, political conflict. The resultant impacts on economic and physical security, freedom, choice and social relations have wide-ranging impacts on well-being and health.
The causal links between environmental change and human health are complex because often they are indirect, displaced in space and time, and dependent on a number of modifying forces. For example, climate changes can place stresses on agricultural production or the integrity of coral reefs and coastal fisheries. This can lead to malnutrition, stunted childhood growth, susceptibility to infectious diseases and other ailments. Deforestation may alter infectious disease patterns, for example by affecting vector (e.g. mosquito) distributions over time. The MA identified key ecosystem services and their links to human health. These are described in more detail below.
Ecosystem services and human health
| Anopheles stephensi mosquito, a known malaria vector, with a distribution from Egypt to China, obtaining a blood meal from a human host. In the wild, mosquito larvae are found in sites such as stream pools and margins, puddles, irrigation channels and springs. In urban areas the larvae are found in a wide variety of artificial containers including cisterns, wells, tubs and fountains. |
Fresh water
Many aspects of the world's hydrological (water) cycle are regulated by the natural functions of ecosystems and associated geophysical processes (such as evaporation and the functioning of the climate system). Human interventions in watersheds, lakes and river systems take many forms - deforestation, farming, irrigation, river damming and extractions from subterranean aquifers. Wetlands play a crucial role in the filtering of fresh water, including the removal of various chemicals and potentially toxic elements (e.g. heavy metals such as cadmium and lead). Fresh water is essential for human health. It is used for growing food, drinking, personal hygiene, washing, cooking and the dilution and recycling of wastes. Water scarcity jeopardizes food production, human health, economic development and geopolitical stability. Globally, the availability of water per person has declined markedly in recent decades. One third of the world's population now lives in countries experiencing moderate to high water stress. This fraction will continue to increase as both population size and per capita water demand grow - reflecting the escalating use of fresh water for irrigated agriculture, livestock production, industry and the requirements of wealthier urban residents. Over 1 billion people lack access to safe water supplies; 2.6 billion people lack adequate sanitation. This has led to widespread microbial contamination of drinking water. Water-associated infectious diseases claim up to 3.2 million lives each year, approximately 6% of all deaths globally. The burden of disease from inadequate water, sanitation and hygiene totals 1.7 million deaths and the loss of more than 54 million healthy life years. Investments in safe drinking-water and improved sanitation show a close correspondence with improvements in human health and economic productivity. Every day each person needs 20-50 litres of water free from harmful chemical and microbial contaminants, for drinking, cooking and hygiene. The growing challenge of providing this basic service to large segments of the human population is highlighted by one of the United Nations Millennium Development Goals, MDG-7, which calls for halving by 2015 the proportion of people without sustainable access to safe drinking-water and basic sanitation.
Food
| Cooking and heating using solid fuels in poorly verticlated houses results in very high levels of exposure to indoor air pollution, especially among women and children. WHO estimates that this causes over 1.6 million deaths per year. |
Productive terrestrial and marine ecosystems, both wild and managed, are the source of our food - a prerequisite for health and life. Global aggregate food production currently is sufficient to meet the needs of all. However, of the present world population of 6.5 billion, over 800 million - nearly all of them in low-income countries - do not obtain enough protein and calories for energy. Worldwide, a similar (increasing) number are now overfed. Several billion people experience deficiences of one or more micronutrients (especially vitamin A, zinc and iodine).
In poor countries, especially in rural areas, the health of human communities often is directly dependent on locally productive ecosystems providing sources of basic nutrition. Local food production is critical in preventing hunger and promoting rural development in areas where the poor do not have the capacity to purchase food from elsewhere. Wild foods are important locally in many developing countries, often bridging the hunger gap created by stresses such as droughts and civil unrest. In richer urban communities, human dependence on ecosystems for food is less apparent but no less fundamental.
Worldwide, undernutrition accounts for nearly 10% of the global burden of disease. Almost all of this occurs in poor countries where food production has not kept up with population increases, particularly in sub-Saharan Africa. Furthermore, undernutrition is related strongly to poverty in developing countries with high mortality rates; between one-sixth and one-quarter of the burden of disease is related to childhood and maternal undernutrition. In developed countries with low mortality rates, diet-related risks (mainly overnutrition, often in combination with physical inactivity) account for between one-tenth and one-third of the burden of disease. The nutritional disparity between rich and poor primarily is caused by social and economic factors as well as the uneven impacts of world food trade. In the future, however, adverse changes in food-producing ecosystems are likely to play an increasingly important role in nutritional disparities (medium certainty).
Timber, fibre and fuel
Many processes and resources in nature provide power that can be harnessed by human communities, especially wind, water and biomass combustion. Different geographical regions and countries at varying stages of development use varied methods of generating power. This has many health impacts and the availability of power, especially electricity, has important applications in health care.
Over half of the world’s population continues to rely upon solid fuels for cooking and heating. These fuels - including wood, crop stubble and animal dung - are a direct product of ecosystems. Indoor air pollution produced by the combustion of biomass fuels as well as coal in poorly ventilated heating and cooking environments, causes significant mortality and morbidity from respiratory diseases, particularly among children. In areas where the demand for wood has surpassed local supply and people cannot afford other forms of power, there is increased vulnerability to illness and malnutrition from consuming (unboiled) microbiologically contaminated water and improperly cooked food, as well as from exposure to cold. Poor women and children in rural communities often are those most affected by a scarcity of fuel wood. Many must walk long distances searching for fuel and firewood (as well as water) and hauling it home. These time-consuming tasks reduce the time and energy available for tending crops, cooking meals or attending school. Therefore, provision of adequate and sustainable energy supplies is fundamental not only to economic development, but also to health and well-being.
Outdoor air pollution is caused predominantly by the combustion of non-renewable fossil fuels for electricity generation, transport and industry. Globally, urban air pollution is responsible for significant mortality every year, mostly as a result of heart and lung diseases. In addition, the accompanying release of a major greenhouse gas (CO2) and its consequent contribution to global warming have further, mostly adverse, impacts on human health. Air pollution due to forest fires and burning practices in agriculture also can have serious local and regional health consequences. This was highlighted by the public health experiences in south-east Asia in 1998, following widespread (drought-associated) forest fires in Sumatra and Kalimantan, Indonesia in the latter part of 1997 and early 1998. Timber exploitation has contributed to species' loss and ecosystem degradation in many regions of the developing world, affecting traditional livelihoods, microbial ecology and causing other health-related risks. In particular the destruction and fragmentation of habitats, accompanied by new patterns of human-microbe contacts, has introduced new infectious diseases into human populations – e.g. the Nipah virus in Malaysia and various viral haemorrhagic fevers in South America. Deforestation also endangers health by intensifying the effects of natural disasters such as floods and landslides (see Box 1.1).
| Bark of whitewillow (Salix alba) was recommended as a pain reliever by the Ancient Greek physician, Hippocrates. Salicin, the active ingredient in willow bark – similarly found in the spirea or meadowsweet plant (Filipendula ulmaria/Spiraea ulmaria) – was discovered in the early 1800s. Aspirin® was introduced to the public in 1899, following synthesis of the salicin derivative: acetylsalicylic acid. |
Biological products
Millions of people around the world depend partly or fully on natural products collected from ecosystems for medicinal purposes. Although synthetic medicines (over half of which originated from natural precursors) are available for many purposes, the global need and demand for natural products persists. Some of the better-known mainstream pharmaceuticals from natural sources include aspirin, digitalis and quinine.
Nutrient and waste management, processing and detoxification
Ecosystems play a critical role in the recycling and redistribution of nutrients. This fundamental service underpins the health of plant and animal species everywhere. Disruption of nutrient cycling can impair soil fertility, resulting in reduced crop yields. This impairs the nutritional status of households (medium certainty) and diet deficiencies (both macro-and micro-nutrients) harm children's physical and mental development. In turn, this can impair the livelihoods of farmers and limit the options open to their children.
Human health can be harmed by exposure to certain toxins produced by algal blooms. These can occur as a result of eutrophication of waterways excessively loaded with nitrates and phosphates infiltrating from run-off water discharged in agricultural, industrial and domestic processes.
Humans are also at risk from inorganic chemicals and persistent organic chemical pollutants in food and water. Such exposures can occur when attempts to improve water access lead to contamination from natural sources (as occurred recently with arsenic contamination of tube wells in Bangladesh), and when human actions release toxic chemicals into the environment (for example, through pesticide use). Toxic chemicals in water and food can have adverse effects on various organ systems. Exposure to low concentrations of some chemicals (such as PCBs, dioxins and DDT) may cause endocrine disruption, interfering with normal human hormonemediated physiology and impairing reproduction.
Regulation of infectious disease
Infectious diseases are caused by viruses, bacteria and other types of microbes or parasites. Only a few infectious agents cause actual disease in plants, animals and humans; usually these are constrained geographically and seasonally by ecosystems and ecological relationships in nature. Patterns of microbe entry into the human species (sometimes as new mutants) are sensitive to climatic and micro-environmental conditions. These factors may impact upon the spread of microbes between humans; their more distant dissemination; and the activity of vector organisms (e.g. mosquitoes) involved in their transmission. Often humaninduced changes in ecosystems and in physical environmental conditions alter these natural influences on infectious agent range and activity.
The pattern and extent of change in incidence of a particular infectious disease depends on the particular ecosystems affected, type of land-use change, disease-specific transmission dynamics, sociocultural changes and the susceptibility of human populations. Infectious disease risks are affected particularly by destruction of, or encroachment into, wildlife habitat (particularly through logging and road building); changes in the distribution and availability of surface waters, e.g. through dam construction, irrigation and stream diversion; agricultural land-use changes, including proliferation of both livestock and crops; uncontrolled urbanization or urban sprawl; resistance to pesticide chemicals used to control certain disease vectors; climate variability and change; migration and international travel and trade; and the accidental or intentional human introduction of pathogens.
| Human health is likely to be affected indirectly by climate-induced changes in the distribution of productive ecosystems. This photo shows rice cultivation in south-east Asia. |
Recently, there has been an upturn in the rate of emergence or re-emergence of infectious diseases. Factors contributing substantially to this trend include: intensified human encroachment on natural environments; reductions in biodiversity (including natural predators of vector organisms); particular livestock and poultry production methods; and increased long-distance trade in wild animal species (including as food). Further contributors include: habitat alterations that lead to changes in the number of vector breeding sites or in reservoir host distribution; niche invasions or interspecies host transfers; human-induced genetic changes of disease vectors or pathogens (such as mosquito resistance to pesticides or emergence of antibiotic-resistant bacteria); and environmental contamination by infectious disease agents.
Cultural, spiritual and recreational services
People and communities obtain many non-material benefits from ecosystems. Ecosystems provide sites and opportunities for tourism, recreation, aesthetic appreciation, inspiration and education. Such services can improve mental health; enhance a subjective sense of culture or place; and also enrich objective knowledge of natural and social sciences, e.g. botany, biology, history and archaeology. Health benefits of these services may be materially less tangible than those captured by conventional health indicators or standard economic valuation measures. Nonetheless, such services are highly valued by people in all societies. Various traditional practices linked to ecosystem services, including seasonal cycles of thanks and celebration, play an important role in developing social capital and enhancing social well-being.
Climate regulation
Regional climatic conditions are influenced by changes in ecosystems and landscapes, especially deforestation and desertification. On a larger scale, the ongoing humaninduced alteration of atmospheric composition (the greenhouse effect) also affects climatic conditions.
Each of the ecosystem services described above is sensitive to climatic conditions and therefore will be affected by human-induced climate change. In turn, these ecosystem changes will affect the well-being and health of human populations. Meanwhile, climate change itself does, and will, affect human health.
Although climate change will have some beneficial effects on human health, most are expected to be negative. Direct effects, such as increased mortality from heatwaves, are most readily predicted but indirect effects are likely to have greater overall impact. Human health is likely to be affected indirectly by climate-induced changes in the distribution of productive ecosystems and in the availability of food, water and energy supplies. These changes will affect the distribution of infectious diseases, nutritional status and patterns of human settlement.
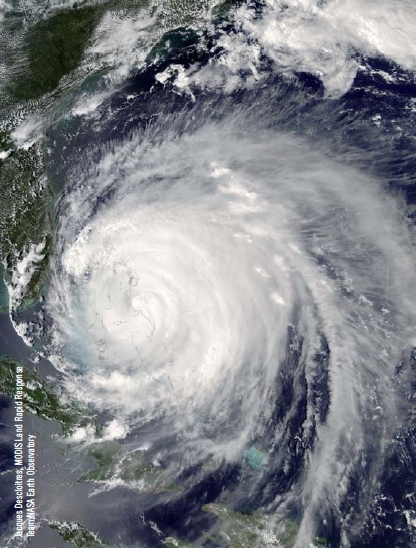
Extreme weather events (including heatwaves, floods, storms and droughts) and sea-level rise are anticipated to increase as a result of climate change. These events have local and sometimes regional effects: directly through deaths and injuries and indirectly through economic disruption, infrastructure damage and population displacement. In turn, this may lead to increased incidence of certain communicable diseases as a result of overcrowding; lack of clean water and shelter; poor nutritional status; and adverse impacts on mental health.
How have ecosystems changed and what are the health implications?
| Extreme weather events, including heatwaves, floods, storms and droughts, are anticipated to increase as a result of climate change. This is a true colour image of Hurricane Frances as it passed over the Bahamas with sustained winds of 185 kph, 3 September 2004. |
As a result of human actions, the structure and functioning of the world's ecosystems changed more rapidly in the second half of the twentieth century than at any other time in human history. The magnitude of these changes is growing as both population size and intensity of economic activity increase. One consequence is that the diversity of life on Earth is being depleted at an accelerating rate. The loss of plant and animal species is irreversible. So, too, is the unravelling or elimination of whole ecosystems.
Human societies also achieve benefits for well-being and health by restructuring and managing various ecosystems. In most countries and regions, the changes made to food-producing ecosystems in recent decades have provided substantial gains in production. Many of the most significant human-induced changes to ecosystems have been essential to meet growing needs for food and water. These changes have helped to reduce the proportion of malnourished people and improve human health.
However, these gains have been achieved at increasing cost: degradation of 60% of ecosystem services; exacerbation of poverty for some; and growing inequities and disparities across groups of people. The intensification of food production methods, expanded use of irrigation, forest-clearing and the intensive exploitation of capture fisheries (e.g. fishing in open marine or inland waters), all have entailed losses in natural resources and changes in ecosystems' functions. The loss from nature of potential medicinal compounds is one consequence. Further, these changes to ecosystems have occurred unevenly, often exacerbating the inequalities in access to ecosystem services and contributing further to poverty. Both within and between countries, poverty is a consistent underlying determinant of undernutrition; lack of access to safe water and sanitation; and lack of access to other public services important to health and well-being, e.g. health services, garbage disposal, etc. These adverse factors have staggering human health implications, costing millions of lives each year.
By dint of much higher per-person consumption levels, the world's richer populations exert disproportionate pressure on global ecosystems - yet are less vulnerable to the adverse consequences. These populations exhibit less vulnerability to the effects of ecosystem degradation, largely as a result of their ability to import resources from, and displace health risks to, other geographical locations.
Poverty and hunger have tended to force rural people onto marginal drought-prone lands with poor soil fertility, and others to urban slums. About 1 billion people are affected by land degradation such as that caused by soil erosion, waterlogging or salinity of irrigated land. Erosion has caused substantially reduced crop yields in Africa.
Diminished human health and well-being tends to increase the immediate dependence on ecosystem services. The resultant additional pressure can (further) damage the ecosystems' capacity to deliver services (medium certainty). As well-being declines, people's options for regulating their use of natural resources at sustainable levels are reduced. Immediate needs inevitably take priority, increasing the pressure on ecosystem services, and can create a downward spiral of increasing poverty and further degradation of ecosystem services.
How might ecosystems change and what would be the health implications?
Continuation of the dual trends of growing exploitation of ecosystem services and the generally declining condition of most ecosystems is unsustainable and likely to lead to irreversible changes. When changes to an ecosystem cross a threshold, recovery is generally slow and costly, even impossible. Thresholds may become lower as anthropogenic impacts simplify these natural systems and reduce their intrinsic resilience to change.
Many of the people and places affected adversely by ecosystem changes and declining ecosystem services are highly vulnerable and ill-equipped to cope with further loss of ecosystem services. Highly vulnerable groups include those whose needs for ecosystem services already exceed supply. This includes people who lack adequate safe water supplies as well as those living in areas with declining agricultural yields and therefore at risk of malnutrition and impaired child development. In tropical and semitropical regions much of the ongoing deforestation alters the dynamics of infectious disease transmission, especially by changing the conditions for mosquito, tick and rodent populations. This may increase outbreaks of diseases such as malaria and dengue fever.
The regions facing the greatest challenges in achieving the MDGs overlap largely with those facing the greatest problems related to the sustainable supply of ecosystem services. Many of these regions include large areas of drylands, in which the combination of population growth and land degradation is increasing human vulnerability to both economic and environmental change and, consequently, impairing well-being and health.
 UNEP/C Jo Kan Sara/TopFoto.co.uk
UNEP/C Jo Kan Sara/TopFoto.co.uk
Ecosystem changes may occur on such a large scale as to have a catastrophic effect on human health. There is an increasing risk of non-linear changes in ecosystems, including accelerating, abrupt and potentially irreversible changes (established but incomplete evidence). The increased likelihood of these non-linear changes stems from the loss of biodiversity and growing pressures from multiple direct drivers of ecosystem change. Similar nonlinearities are anticipated in social-economic-political contexts. For example, widespread food insecurity resulting from severe climate change, institutional failure and increasingly damaged soils could worsen inequality and lead to widespread conflict. Meanwhile, a great many individually less dramatic losses in ecosystem services are likely to influence human health adversely. The MA Scenarios Working Group developed four scenarios to explore possible future trends and developments until 2050, and the consequences for ecosystem services and human well-being. Scenarios are plausible, proactive and relevant stories about how the future might unfold. They are not forecasts, projections, predictions or recommendations. Rather, they are implications of specific policy outcomes based on current knowledge of underlying socioecological processes. The MA scenarios are used to explore a range of contexts under which sustainable development could be pursued, and approaches supporting sustainable development. The scenarios are: (i) Global Orchestration: globally-driven economic development emphasising social responsibility, equity, and social public goods, and with a reactive approach to ecosystems; (ii) Order from Strength: regionalized development with an emphasis on security and economic growth and a reactive approach to ecosystems; (iii) Adapting Mosaic: regionalized development emphasising proactive management of ecosystems, local adaptation and flexible governance; and (iv) TechnoGarden: globalized development using technology to achieve environmental outcomes, with a proactive approach to ecosystems (see Box 3.2).
Under all four MA scenarios, the projected changes in the underlying driving forces result in significant growth in consumption of ecosystem services, continued loss of biodiversity and further degradation of some ecosystem services.
- During the next 50 years, demand for food is projected to grow by 70-80% and demand for water by 30-85%. Water withdrawals in developing countries are projected to increase significantly.
- Food security is not achieved under any of the MA scenarios by 2050. Child malnutrition will be difficult to eliminate, despite an increasing food supply and more diversified diets.
- A severe deterioration of the services provided by freshwater resources (such as aquatic habitat; fish production; water for households, industry and agriculture) is found in the scenarios that are reactive to environmental problems. Less severe but still important declines are expected in the scenarios that are more proactive about environmental problems.
- Habitat loss and other ecosystem changes are projected to lead to a decline in local diversity of native species by 2050.
In the scenarios with more promising health prospects, the number of undernourished children is reduced and the burden of epidemic diseases such as malaria and tuberculosis also falls. Improved vaccine development and distribution could allow populations to cope relatively well with the next influenza pandemic, while the impact of other new infectious diseases should also be limited if wellcoordinated public health measures are in place. Under a less optimistic scenario, the number of malnourished children increases. The health and social conditions for rich and poor countries diverge and a negative spiral of poverty, declining health and degraded ecosystems could develop.
What actions would address the health consequences of ecosystem change?
|
|
| Improving water and sanitation infrastructure in Viet Nam, (UNEP/Dinh Tran/TopFoto.co.uk) |
==
There are two strategies for avoiding disease and injury caused by ecosystem disruption. One - preferable in principle - is to prevent, limit or manage the environmental damage. The other is to make adaptive changes that will protect individuals and populations from the adverse consequences of ecosystem change. These should not be viewed as alternatives; both strategies are useful. Two aspects need to be considered to understand the potential negative health impacts of ecosystem change: the current (and likely future) intrinsic vulnerability (e.g. nutritional status) of populations and their likely future capacity for adaptation. These are closely related. In many cases the forces that place populations at risk (such as poverty and high burdens of disease) also impair their capacity to prepare for the future.
As part of a strategy for achieving the MDGs, improved ecosystem management would need to address a complex set of underlying causes of environmental change. This entails cross-sectoral policies, institutions and investments on local, national, regional and global scales. Achievement of the MDGs, enhanced human well-being and improved human health status requires particular attention to improving ecosystem management and the capacity for policy-making at national and local levels. Meanwhile, there is the need to address global challenges including long-term climate change, the depletion of international fisheries and the spread of exotic species.
How can priorities be established for actions to address the health consequences of ecosystem change?
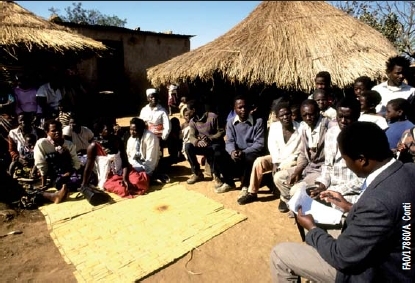
| Monitoring nutritional status in Zambia: an officer from the Central Statistical Office collects data on food and water availability and prices of important food items in a village. |
There is a need for a more systematic inventory, by region and country, of current and likely population health impacts of ecosystem change. Clearly, information is a crucial resource. An appropriate metric - for instance disability-adjusted life years (DALYs) gained or lost - should be used to make at least approximate estimates of these impacts. This will require an unusual level of interdisciplinary analysis and synthesis in which the population health sciences are central, especially epidemiology. Burdenof- disease evaluations within the context of ecosystem change are appropriate for aggregating health impacts through a range of mechanisms and, potentially, can aid priority-setting and decision-making to address ecosystem change. However, they must be considered as only one component of evidence; they cannot account fully for complex causal pathways, long timescales and potential irreversibility. These important properties need to be included in the final considerations about any response to ecological change.
Priority-setting of actions to address the health consequences of ecosystem change also should reflect the priorities and values of all those affected by the proposed actions. Therefore the final decisions about priorities should be taken either by individuals or by their legitimate political representatives, with reference to the prevailing stakeholder/community values.
It is important to consider which sections of the population are most affected by ecological changes, including the distribution of disease impacts by age, gender, social status, ethnicity and geographical region. Global estimates for the year 2000 indicated that in poor countries with high mortality rates, between one-sixth and one-quarter of the total disease burden was attributable to childhood and maternal undernutrition. Children and pregnant women are at much greater risk for morbidity and mortality from malaria, particularly if malnourished; morbidity and mortality due to heatwaves is highest among the elderly. Many other such differences in vulnerability to disease have been documented. For example, in many poor countries the risk of child diarrhoeal disease is related strongly to poverty and the risk of malnutrition among the poor is greater among girls than among boys.
The responses to ecosystem changes include mitigation and adaptation. Mitigation implies reducing or reversing the change process. Adaptation aims to increase the resilience of both social systems and ecosystems to the impacts of ecosystem change in order to reduce the current and future health risks – and to take advantage of beneficial consequences of ecosystem changes. Decisions on priority actions should consider the best evidence available on the likely effectiveness of any intervention in either class. Mitigation and adaptation response options can be legal, economic, financial, institutional, social, behavioural, technological or cognitive. They encompass spontaneous responses to ecosystem change and planned (anticipatory) interventions by affected individuals and institutions such as governments. In order to protect human health, responses very often must involve actions outside of the health sector – particularly in agriculture, industry, education, coastal zone management and urban planning.
What are the policy implications of ecosystem change's threats to health?
Measures to ensure ecological sustainability would safeguard ecosystem services and thereby benefit health in the long term. A good and equitable health status within a population confers a range of social, economic and political benefits. Society is more cohesive, more productive and more stable. For a population weighed down by disease related to poverty and by inequities in access to food and other resources, equitable provision of these resources would have major health benefits (high certainty). Where ill-health is caused, directly or indirectly, by excessive consumption of ecosystem services (such as food and energy), substantial reductions in consumption would have major health benefits and simultaneously reduce pressure on life-support systems (high certainty).
Increasing populations and growing economies result in higher total consumption. In addition to the pressure on ecosystems this situation directly increases certain health risks - such as those from over-nutrition and physical inactivity. A reduction in consumption of animal products and refined carbohydrates (simple sugars) in rich countries would have benefits for both human health and ecosystems. The rise of obesity in urban populations around the world is essentially a 'human ecological' problem due to the societallevel imbalance between energy ingested and energy expended - it is a modern way-of-living problem. The implementation of better transport practices and systems could lead to fewer injuries, decreases in obesity and cardiovascular disease through more physical activity in sedentary populations, and reductions in local air pollution and greenhouse gas emissions. Integration of national agricultural and food security policies with the economic, social and environmental goals of sustainable development could be achieved, in part, by ensuring that the environmental and social costs of production and consumption are reflected more fully in the market price of food and water.
Cross-sectoral policies that promote ecologically sustainable development and address underlying driving forces also will be essential. Agenda 21, the international action plan adopted in 1992 at the United Nations Conference on Environment and Development (Earth Summit), and the World Summit on Sustainable Development Plan of Implementation, adopted in Johannesburg in 2002, both describe a comprehensive approach to ecologically sustainable development incorporating cross-sectoral policies. Within these two frameworks, the following strategies have specific relevance to health.
- Mitigation strategies that reduce the underlying causes of ecosystem change, while simultaneously improving human health.
- Adaptation strategies to reduce the effect of ecosystem disruption on health (addressing direct, mediated and long-term health impacts).
- Integrated action for health, such as a health impact assessment of major development projects, policies and programmes and indicators for health and sustainable development.
- Inclusion of health in sustainable development planning efforts such as Agenda 21, in multilateral trade and environmental agreements and poverty reduction strategies.
- Improvement of intersectoral collaboration between different tiers of government, government departments and NGOs.
- International capacity-building initiatives that assess health and environment linkages, using the knowledge gained to create more effective national and regional policy responses to environmental threats.
- Dissemination of knowledge and good practice on health gains from intersectoral policy.
The ongoing degradation of ecosystem services is a significant barrier to achieving the MDGs. Ecologically unsustainable use of ecosystem services raises the potential for serious and irreversible ecological change. This may occur on such a large scale as to have a catastrophic effect on the economic, social and political processes on which social stability, human well-being and good health depend. The MDGs give prominence to achieving reductions in malnutrition, infectious diseases, maternal mortality, exposure to unsafe drinking-water and, most importantly, poverty. All these goals are seriously jeopardized by continuing decline in the world's ecosystems. This indicates strongly that a precautionary approach to environmental protection is the most effective way to protect and enhance health. Unavoidable uncertainties about aspects of the risks to well-being and health from environmental changes should not be an excuse for delaying policy decisions.
Terms of Use
The copyright for material on this page is the property of the World Health Organization. Click here for the Terms of Use (Ecosystems and Human Well-being: Health Synthesis: Summary for Decision-Makers).
Disclaimer: This chapter is taken wholly from, or contains information that was originally written for the Millennium Ecosystem Assessment as published by the World Health Organization. The content has not been modified by the Encyclopedia of Earth.
|
|