Brucellosis
Contents
- 1 Introduction (Brucellosis)
- 1.1 U.S. Geological Survey
- 1.2 Centers for Disease Control and Prevention
- 1.2.1 What is brucellosis?
- 1.2.2 How common is brucellosis?
- 1.2.3 Where is brucellosis usually found?
- 1.2.4 How is brucellosis transmitted to humans, and who is likely to become infected?
- 1.2.5 Can brucellosis be spread from person to person?
- 1.2.6 Is there a way to prevent infection?
- 1.2.7 My dog has been diagnosed with brucellosis. Is that a risk for me?
- 1.2.8 How is brucellosis diagnosed?
- 1.2.9 Is there a treatment for brucellosis?
- 1.2.10 I am a veterinarian, and I recently accidentally jabbed myself with the animal vaccine (RB-51 or strain 19, or REV-1) while I was vaccinating cows (or sheep, goats). What do I need to do?
- 2 References
- 3 Further Reading
Introduction (Brucellosis)
U.S. Geological Survey
Wildlife Health Connection to Emerging Infectious Diseases
"Wildlife, domestic animals and humans share a large and increasing number of infectious diseases. The continued globalization of society, human population growth, and associated landscape changes will further enhance interfaces between wildlife, domestic animals, and humans, thereby facilitating additional infectious disease emergence. These interfaces are such that a century-old concept of “the one medicine” is receiving greater attention because of the need to address these diseases across species if their economic, social, and other impacts are to be effectively minimized. The wildlife component of this triad has received inadequate focus in the past to effectively protect human health as evidence by such contemporary diseases as SARS, Lyme disease, West Nile Fever, and a host of other emerging diseases. Further, habitat loss and other factors associated with human-induced landscape changes have reduced past ability for many wildlife populations to overcome losses due to various causes. This, disease emergence and resurgence has reached unprecedented importance for the sustainability of desired population levels for many wildlife populations and for the long-term survival of some species"[1]
Centers for Disease Control and Prevention
The Centers for Disease Control and Prevention has prepared answers to frequently asked questions about Brucellosis, and about the organism that causes this disease:
What is brucellosis?
 Brucella spp. (Source: Centers for Disease Control and Prevention; Credit: Larry Stauffer, Oregon State Public Health Laboratory)
Brucella spp. (Source: Centers for Disease Control and Prevention; Credit: Larry Stauffer, Oregon State Public Health Laboratory) Brucellosis is an infectious disease caused by the bacteria of the genus Brucella. These bacteria are primarily passed among animals, and they cause disease in many different vertebrates. Various Brucella species affect sheep, goats, cattle, deer, elk, pigs, dogs, and several other animals. Humans become infected by coming in contact with animals or animal products that are contaminated with these bacteria. In humans brucellosis can cause a range of symptoms that are similar to the flu and may include fever, sweats, headaches, back pains, and physical weakness. Severe infections of the central nervous systems or lining of the heart may occur. Brucellosis can also cause long-lasting or chronic symptoms that include recurrent fevers, joint pain, and fatigue.
How common is brucellosis?
Brucellosis is not very common in the United States, where100 to 200 cases occur each year. But brucellosis can be very common in countries where animal disease control programs have not reduced the amount of disease among animals.
Where is brucellosis usually found?
Although brucellosis can be found worldwide, it is more common in countries that do not have good standardized and effective public health and domestic animal health programs. Areas currently listed as high risk are the Mediterranean Basin (Portugal, Spain, Southern France, Italy, Greece, Turkey, North Africa), South and Central America, Eastern Europe, Asia, Africa, the Caribbean, and the Middle East. Unpasteurized cheeses, sometimes called "village cheeses," from these areas may represent a particular risk for tourists.
How is brucellosis transmitted to humans, and who is likely to become infected?
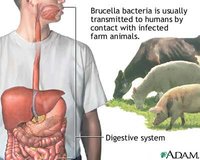 Brucella transmission. (Source: National Institutes of Health / National Library of Medicine).
Brucella transmission. (Source: National Institutes of Health / National Library of Medicine). Humans are generally infected in one of three ways: eating or drinking something that is contaminated with Brucella, breathing in the organism (inhalation), or having the bacteria enter the body through skin wounds. The most common way to be infected is by eating or drinking contaminated milk products. When sheep, goats, cows, or camels are infected, their milk is contaminated with the bacteria. If the milk is not pasteurized, these bacteria can be transmitted to persons who drink the milk or eat cheeses made it. Inhalation of Brucella organisms is not a common route of infection, but it can be a significant hazard for people in certain occupations, such as those working in laboratories where the organism is cultured. Inhalation is often responsible for a significant percentage of cases in abattoir employees. Contamination of skin wounds may be a problem for persons working in slaughterhouses or meat packing plants or for veterinarians. Hunters may be infected through skin wounds or by accidentally ingesting the bacteria after cleaning deer, elk, moose, or wild pigs that they have killed.
Can brucellosis be spread from person to person?
Direct person-to-person spread of brucellosis is extremely rare. Mothers who are breast-feeding may transmit the infection to their infants. Sexual transmission has also been reported. For both sexual and breast-feeding transmission, if the infant or person at risk is treated for brucellosis, their risk of becoming infected will probably be eliminated within 3 days. Although uncommon, transmission may also occur via contaminated tissue transplantation.
Is there a way to prevent infection?
Yes. Do not consume unpasteurized milk, cheese, or ice cream while traveling. If you are not sure that the dairy product is pasteurized, don't eat it. Hunters and animal herdsman should use rubber gloves when handling viscera of animals. There is no vaccine available for humans.
My dog has been diagnosed with brucellosis. Is that a risk for me?
B. canis is the species of Brucella species that can infect dogs. This species has occasionally been transmitted to humans, but the vast majority of dog infections do not result in human illness. Although veterinarians exposed to blood of infected animals are at risk, pet owners are not considered to be at risk for infection. This is partly because it is unlikely that they will come in contact with blood, semen, or placenta of the dog. The bacteria may be cleared from the animal within a few days of treatment; however re-infection is common and some animal body fluids may be infectious for weeks. Immunocompromised persons (cancer patients, HIV-infected individuals, or transplantation patients) should not handle dogs known to be infected with B. canis.
How is brucellosis diagnosed?
Brucellosis is diagnosed in a laboratory by finding Brucella organisms in samples of blood or bone marrow. Also, blood tests can be done to detect antibodies against the bacteria. If this method is used, two blood samples should be collected 2 weeks apart.
Is there a treatment for brucellosis?
Yes, but treatment can be difficult. Doctors can prescribe effective antibiotics. Usually, doxycycline and rifampin are used in combination for 6 weeks to prevent re-occuring infection. Depending on the timing of treatment and severity of illness, recovery may take a few weeks to several months. Mortality is low (<2%), and is usually associated with endocarditis.
I am a veterinarian, and I recently accidentally jabbed myself with the animal vaccine (RB-51 or strain 19, or REV-1) while I was vaccinating cows (or sheep, goats). What do I need to do?
These are live vaccines, and strain 19 is known to cause disease in humans. Although we know less about the other vaccines, the recommendations are the same. You should see a health care provider. A baseline blood sample should be collected for testing for antibodies. We recommend that you take antibiotics (doxycycline and rifampin for strain 19 and REV-1, or doxycycline alone for RB-51) for 3 weeks. At the end of that time you should be rechecked and a second blood sample should be collected. (The sample can also be collected at 2 weeks.) The same recommendations hold true for spraying vaccine in the eyes (6 weeks of treatment in this case) or spraying onto open wounds on the skin.
Date: December 7, 2007
References
^ Milton Friend, USGS Emeritus Scientist. Founding Director, USGS National Wildlife Health Center.