Specific and Management Diseases
 |
Specific and Management Diseases
|
In this section is listed the diseases that are to a large extent management and environment related, such as diarrhea, bloat, FMD, foot problems and mastitis, but also mention signs to look for the disease Rinderpest, which has now been declared extinct in East Africa, so that in case it resurfaces, there will be at least reference material. Also Nairobi sheep disease, PPR and Plant and other Poisoning are included here.
|
Local names:
Luo: ich-kuot / Embu: nunvita / Gabbra: furfur / Gikuyu: huhita / Kamba: kwimbanywa / Kipsigis: kowiren / Maasai: Embo'ngit, Ediis, empomgit / Maragoli: kuhaata, myika munda/ Meru: mpwna / Samburu: mberini / Somali: bakhakh, dunbudhyo, balao, baalallo, dhibir, dibiyio / Turkana: lotebwo, akitebukin, akiurur / Pokot: lesana /
Other name: Ruminal Tympany
|
|
|
Introduction
With the onset of long rains, livestock keepers, especially goat, sheep and cattle keepers should become aware of the dangers of bloat to their livestock. Bloat occurs when there is an abrupt nutritional change in the diet and especially when ruminants feed on lush green pastures. It simply means animals have too much gas in their stomach.
How animals get bloat
The rumen of cattle, sheep and goats is like a large container in which a mixture of partly digested feed and liquid is continuously fermenting, producing large quantities of gas. For example, an average cow can produce over a thousand litres of gas in a day. Some of the gas is removed by absorption into the blood stream but most of it is removed by belching during "cudding". If the gas cannot escape, the rumen literally "blows up" and the animal gets bloat. It can happen when:
- Animals eat too many legumes or too much fresh, lush grass (e.g. olenge grass (Luo))
- Animal eats too much grain (e.g. finger millet, Acacia pods)
- Animal eats cassava leaves or peels
- Something blocks the passage of food in the stomach or gullet
Types of bloat
There are two types of bloat: Frothy Bloat and Free Gas Bloat.
Animals get Frothy Bloat when the rumen becomes full of froth (foam). Several animals in the herd may get this type of bloat at the same time when they graze on wet, green pasture mixed with legumes in the field. Foaming substances are found in certain plants such as legumes of which lucerne, clover and young green cereal crops are examples.
Frothy Bloat is due to the production of a stable foam, which traps the normal gases of fermentation in the rumen. Pressure increases because belching cannot occur. Initially the distension of the rumen stimulates rumen movements, which makes the frothiness even worse. Later on because of the distension there is loss of muscle tone and loss of the rumen's ability to move spontaneously, compounding the situation.
Saliva has antifoaming properties. More saliva is produced when food is eaten slowly than when it is eaten quickly. Succulent forages are eaten more rapidly and digested more quickly and as a result less anti-foaming saliva is produced. Grazing on immature, lush, succulent, rapidly growing pastures with a high concentration of soluble proteins is most conducive to bloat, as is the stage of growth of the plant, not its degree of wetness.
Causes of Frothy Bloat
- The primary cause of frothy bloat appears to be a change in the composition of certain pasture plants, the change being one that facilitates the development of a stable foam that in turn prevents belching
- Frothy Bloat normally happens at the start of wet season when the diet of grazing animals abruptly changes from dry feeds to wet lush pastures that contains some legumes.
- Animals also get Frothy Bloat when they feed on ripe fruits or other feeds that ferment easily.
- Some poisonous plants can cause sudden and severe bloat.
- A sudden change in the type of food can also cause Frothy Bloat.
- Frothy bloat can also occur in feedlots with insufficient roughage, or food too finely ground. This leads to a shortage of rumen-stimulating roughage, and prevents the rumen's ability to move spontaneously and hinders belching and release of gas.
Free Gas Bloat is usually due to physical obstruction of the oesophagus, often by a foreign body such as a potato, avocado, apple etc. Grain overload leading to stopping of of normal rhythmic contractions of the rumen wall can also cause this type of bloat as can unusual posture, particularly lying down, as may occur in a cow affected by milk fever. This type of bloat normally only affects one or two animals in the herd at the same time, not several as in the case of Frothy Bloat. As the name suggests, in this type of bloat the gas lies above the food in the rumen and is not mixed with it, as it is in Frothy Bloat.
Signs of Bloat
- The left side of the abdomen behind the ribs becomes very distended and very tense, like a drum. Later the right side also becomes distended
- The animal stops eating
- The animal may grunt and have difficulty in breathing
- There may be mouth breathing
- The animal may stamp its feet on the ground
- Sometimes green froth comes out of the mouth and nose
- There may be extension of the tongue from the mouth
- Diarrhoea is common in cases of Frothy Bloat
- Animals may collapse and die after only an hour or so
- There is often frequent urination
Prevention - Control - Treatment
Prevention of bloat
1. Feed the animals with dry grass or hay to fill them up before you turn them out onto new wet lush pasture. For this to be effective the hay or dry grass should form at least one third of the diet.
2. Do not water the animals just before you put them on to wet pasture
3. Do not graze the animals on wet green pasture early in the morning. Wait until the pasture has been dried up by the heat of the morning sun
4. You should gradually increase the grazing hours of the animals on wet green pasture over the first week. Do not put the animals out all day and leave them there.
5. Avoid abrupt changes in the diet of animals and always give newly introduced feeds in small quantities.
6. If possible try to strip graze animals to reduce intake and to maintain grass dominance in the stretch of grass. The pasture ideally should have at least 50% grass.
7. During the risk period the continual administration of anti-foaming agents such as Stop Bloat should be considered.
8. Watch animals closely at all times during the risk period.
9. Keep anti-foaming agents close at hand during the risk period.
10. In feedlot or zero grazing situations rations must contain 10-15% chopped roughage mixed into the complete diet. This should be a cereal, grain straw, grass hay or equivalent. Grains should be rolled or cracked, not finely ground.
Treatment of bloat
Depending on the type of bloat, several methods of treatment can be applied:
- Do not feed the animal for a few hours and make the animal move around (remember it can die within 1 hour if the bloat is severe)
- For less severe cases of frothy bloat, give 500ml to large animals and 100ml to small animals of any edible vegetable oil, solid cooking oil, butter oil, ghee or milk orally (by mouth). Non-toxic mineral oils can also be used effectively.
- Severe bloat is an emergency and rapid action is required to save the animal's life. In life-threatening cases where the animal can not breathe, an emergency rumenotomy may be necessary. Puncture carefully the skin and the rumen of the animal on the left flunk to let the gas out. Use a knife or any sharp thing but the best instrument to use is the trochar and cannula. The hole should be made at a hands' width behind the last rib and a hand away from the edge of the backbone. Push hard because the skin is very tough. Gas and froth will come out when you make the hole. It helps to put a tube or cannula through the hole to keep the hole open. There will be an explosive release of gas and rumen contents. Remember that in severe cases if this is not done the animal will die. SO DO IT .
- Pour some vegetable oil into the rumen through the hole to help stop further gas or froth formation. Complications are rare. Call a veterinarian to attend to a punctured abdomen or a difficult case of bloat.
- Another aid is to tie a stick in the mouth to stimulate the flow of saliva, which is alkaline and helps to denature the foam.
- Forceful walking may help to coalesce the foam into larger bubbles and stimulate belching.
- Give bloat medicine such as the following: Stop Bloat, Bloat Guard or Birp once daily for 3 days
- In cases of Free Gas Bloat due to a foreign body lodged in the oesophagus, it may have to be dislodged by using a probang or stomach tube, for which the services of a veterinarian will be required.
Common traditional practice
Some of the following practices may have some merit in case of emergencies where no vegetable oil is available:
- Gabbra: Mix 4 teaspoons of laundry detergent with 1 litre of milk. Drench 1 litre for an adult cow (0.5 litre for sheep and goats)
- Turkana: Mix 500g Magadi soda with 1 litre of water. Stir well and drench adult cattle with the mixture. For calves, goats and sheep use 0.5 litre. For large camels give 2 litres.
- Luo: Mix 0.5 litre of paraffin oil with a handful of olulusia (Vernonia amygdalina) leaves and 2 spoons of salt. Drench with half this amount.
- Kamba: Mix a handful of wood ash with 1 soda bottle (300ml) of water. Sieve and drench adult cattle with this amount. Use half the amount for calves, sheep and goats.
(Source:ITDG and IIRR 1996)
Local names:
Luo: diep nyaroya / Kikuyu: ruharo rwa kimira / Maasai: Iinkati /
Luo: diep nyaroya / Kikuyu: ruharo rwa kimira / Maasai: Iinkati /
Common names: Bovine virus diarrhoea
Description: Management disease
Introduction
Mucosal Disease is caused by the same virus which causes Bovine Viral Diarrhoea. Both are manifestations of infection by the same virus. At one time it was thought that these were two separate diseases. Mucosal Disease refers to the condition in cattle persistently infected with inactive BVD virus when they become superinfected with active virus and develop clinical disease.
Incidence is low but mortality is high. The virus occurs all over the world and is probably more widespread than most people think, even in Kenya. Cattle that are infected persistently (insert dictionary) with inactive Bovine Viral Diarrhoea Virus serve as a natural reservoir of virus.
Mode of spread
Transmission can occur after birth by contact with infected secretions and excretions shed by persistently infected animals. Needle transmission can occur. Pre-natal (transmission to the calf before birth) persistent infection develops when inactive virus is transmitted through the placenta during the first 4 months of foetal development. The calf is born infected and remains infected for life. Infection through the placenta later in gestation results in abortion, congenital malformations, or birth of normal calves that have antibody against BVDV, so the outcome of infection varies according to the stage of pregnancy when infection occurs.
Transmission can occur after birth by contact with infected secretions and excretions shed by persistently infected animals. Needle transmission can occur. Pre-natal (transmission to the calf before birth) persistent infection develops when inactive virus is transmitted through the placenta during the first 4 months of foetal development. The calf is born infected and remains infected for life. Infection through the placenta later in gestation results in abortion, congenital malformations, or birth of normal calves that have antibody against BVDV, so the outcome of infection varies according to the stage of pregnancy when infection occurs.
Up to 90 days of pregnancy
At this stage infected cows give birth to a calf with permanent infection of the disease and whose immune system does not recognize the virus as a foreign organism ("anti body negative calves"). Fifty percent of these calves develop clinical disease and die within the first two years Calves appear to be stunted, and prone to respiratory and intestine ailments. In the infected mother foetal death and irregular returns to service occur.
At this stage infected cows give birth to a calf with permanent infection of the disease and whose immune system does not recognize the virus as a foreign organism ("anti body negative calves"). Fifty percent of these calves develop clinical disease and die within the first two years Calves appear to be stunted, and prone to respiratory and intestine ailments. In the infected mother foetal death and irregular returns to service occur.
90 to 180 days of pregnancy
Infection at this stage causes abortion or the birth of a congenitally deformed calf with perhaps eye and brain abnormalities or a persistently infected calf possibly with some antibody.
Infection at this stage causes abortion or the birth of a congenitally deformed calf with perhaps eye and brain abnormalities or a persistently infected calf possibly with some antibody.
After 180 days of pregnancy
At this stage, the immune system of the foetus is fully developed and the immune system of the foetus detects and clears itself of infection. At birth such calves are normal and have antibodies against the disease. But abortion may still occur in the mother.
At this stage, the immune system of the foetus is fully developed and the immune system of the foetus detects and clears itself of infection. At birth such calves are normal and have antibodies against the disease. But abortion may still occur in the mother.
Whatever the stage of pregnancy the cow herself will often be only mildly affected - she may have a raised temperature and scour for a few days but only occasionally develops a severe illness. It is the persistently infected calf which causes problems.
Signs of Bovine Viral diarrhea
- BVDV is immunosupressive and as as result an infected animal is much more susceptible to other infections such as those affecting the gut or lungs
- The virus attacks all the mucosal surfaces in the body causing inflammation and ulceration and it is the results of this which cause the symptoms seen.
- Erosions can occur throughout the intestinal tract, lesions are seen in the mouth, nose and muzzle, there is often foul smelling diarrhoea containing shreds of intestine, mucus and blood.
- Occasionally diarrhoea may be so severe as to appear like water or paralysis of the gut may occur with no sign of faecal material.
- Other signs which may occur include discharges from the nose, excessive tears and lameness due to eruptive lesions of the interdigital cleft and coronary band.
- Animals are reluctant to eat and there is drooling and even frothing from the mouth.
- High mortality with moderate morbidity (the ratio of sick to well animals) is to be expected.
- In Mucosal Disease, where a persistently infected animal, usually under 2 years of age, is superinfected with internally acquired active virus, the mortality is very high, death occurring within a few days of onset, with fever, dysenteric diarrhoea, lack of appetite, dehydration, ulceration throughout the gastro-intestinal tract and erosive lesions in the mouth and nose.
Diagnosis
- Diagnosis is based on the disease history, clinical signs, gross and microscopic lesions, virus isolation from tissues such as spleen, thyroid and salivary gland and examination of paired serum samples when a more than four- fold increase in antibody titre indicates recent infection.
- Difficulties may occur when the presenting animal has no specific neutralising antibody due to immunesuppression or the inability to secrete antibody. So the whole picture must be considered.
- For diagnosis serum samples have to be sent to a laboratory outside of Kenya.
Suspect BVD when you see:
- The birth of congenitally abnormal calves,
- unexplained abortions,
- the appearance of stunted ill calves in the herd and
- cases of severe diarrhoea in young animals under the age of two years followed by their death must arouse a suspicion of BVD/ Mucosal Disease.
- There will be a low incidence (5%) of acute clinical disease but a high case mortality.
Prevention - Control - Treatment
- Treatment is limited to supportive therapy such as providing antibiotic cover to prevent secondary bacterial infections, appetite stimulants, vitamins and alimentary tract astringents, such as kaolin, charcoal etc.
- Post-natally acquired BVD virus infections are trivial. Control measures therefore are directed to limiting the risk of transplacental infection.
- Persistently infected animals should be identified and removed and isolated from the breeding herd. Only virus-negative and antibody-positive animals should be retained in the herd.
- Live and killed vaccines have been developed. The former has several disadvantages such as the risk of transplacental infection, they are immunosuppressive and epidemics of the mucosal disease syndrome have been recorded after their use. Killed vaccines are safe, but booster doses are necessary to achieve a good level of protected immunity.
- Because the disease mainly affects cattle under 2 years and since colostral immunity from BVD positive cows wanes by 6 months of age the vaccination of young stock between 6 months and 2 years of age is a logical approach - but the manufacturer's instructions should always be followed.
- Vaccine is obtainable from the UK and the US
Local names:
Embu: kuvarua / Gabbra:halabata, albahti, albata / Luo: Ambululu, diep / Kipsigis:keburketan / Kikuyu: ruharo,kuharuo / Kamba:wituuo / Maasai: Ankorotik, olodo kurum / Maragoli: kunyalala munda / Samburu: ngorotit, nkiriato, ngiriata, kep-ngochek / Somali: har, har dig, hardik, shutan, daab, adeya / Turkana: eremonu, lomaritenit, anemoriloleo, lolera /
Embu: kuvarua / Gabbra:halabata, albahti, albata / Luo: Ambululu, diep / Kipsigis:keburketan / Kikuyu: ruharo,kuharuo / Kamba:wituuo / Maasai: Ankorotik, olodo kurum / Maragoli: kunyalala munda / Samburu: ngorotit, nkiriato, ngiriata, kep-ngochek / Somali: har, har dig, hardik, shutan, daab, adeya / Turkana: eremonu, lomaritenit, anemoriloleo, lolera /
Description:
Management disease
Introduction
Many diseases of young animals can be controlled with proper hygiene and health management. Although calves will inevitably be exposed, minimizing risk factors will result in fewer infections and illness in calves.
Diarrhoea is a common disease in livestock - calves, lambs and kids- , especially in the newborn and suckling young animals. The acute disease in the newborn is characterised by progressive dehydration and rapid death, sometimes in as few as12 hours. In the subacute form, diarrhoea may persist for several days and result in emaciation and stunted growth.
Diarrhoea is a common disease in livestock - calves, lambs and kids- , especially in the newborn and suckling young animals. The acute disease in the newborn is characterised by progressive dehydration and rapid death, sometimes in as few as12 hours. In the subacute form, diarrhoea may persist for several days and result in emaciation and stunted growth.
Causes
Several pathogens are associated with neonatal diarrhoea. The most common are the bacterium Escherichia coli, the viruses (Rota and Corona) and Cryptosporidia parasites. Others include Salmonella, Clostridia and Giardia. The organisms responsible for diarrhoea are commonly found in the faeces of healthy animals but they can also come from the pen or from the boma and from dirty foul standing water. A few calves with diarrhoea can result in severe contamination of the calf rearing area. Transmission to younger calves is directly by mouth. Close contact between calves facilitates transmission of disease. Do not place calf pens close together.
Diarrhoea can also occur because of stress, dirty housing, overcrowding, feeding dirty milk or feeding too much milk.
Contaminated feed can be a serious source for Salmonella infection.
Diarrhoea can also occur because of stress, dirty housing, overcrowding, feeding dirty milk or feeding too much milk.
Contaminated feed can be a serious source for Salmonella infection.
Signs of Diarrhoea
- Bad smelling soft, sometimes watery, faeces which is usually whitish in color and sometimes frothy. In older calves, the color of the dung is darker.
- The affected calves lack appetite, becomes dull and refuse to drink.
- The calf develops fever and loses water, minerals and energy very fast until it canot stand up any more.
- The skin of the calf becomes dry and looses elasticity. If you raise a skin fold it remains standing for a while and does not move back. This is a sign of severe dehydration.
- Also the mouth of the calf beocme cold and the eyes sink into the socket.
- Calves that are dull, have a cold mouth and a dry skin and cannot stand may die very fast.
The major symptoms of diarrhoea are dehydration (lack of water), profound weakness, and death within one to several days of onset. Onset is sudden with passing of a lot of liquid faeces.The calf rapidly becomes depressed because of loss of fluids, salt and energy. It becomes too weak to stand. Death may occur in severe cases within 12 - 24 hours.
Salmonella infections usually occur in calves older than 14 days and can also affect weaners. The faeces are often foul smelling, and contain blood, clots and mucous. There is general infection (septicaemia ) with high fever, and depression leading to collapse and coma. Affected calves lose weight rapidly and often die despite treatment with antibiotics.
Clostridial diarrhoea affects calves/lambs/kids of a few days old, which are strong and have good appetite. Onset is sudden with depression, weakness, bloody diarrhoea, abdominal pain and death within a few hours. Clostridia produce a lot of toxin which kills very fast. Most die before treatment can be started.
Viral infections such as those due to Rotavirus or Coronavirus affect calves of 5 - 15 days old but can affect older calves up to several months of age. Most are only moderately depressed and continue to suck and drink milk. The faeces are soft to liquid, and often contain large amounts of mucous. The diarrhoea often persists for several days. Response to fluid and electrolyte therapy and nutritional support is usually very good.
Cryptosporidiosis occurs most commonly in the second week of life, with persistent diarrhoea which does not respond to treatment. Often it is mild and self limiting but if mixed with other organisms may be severe and life-threatening.
Coccidiosis causes diarrhoea in young calves/kids/lambs but also in older animals up to weaning age. They are unthrifty, faeces are thin watery with blood. Faeces look red at first and then become dark. Calves often press trying to pass faeces. They may be depressed, not eat and become dehydrated.
Dietary diarrhoeas occur in calves less than 3 weeks old and shows pasty faeces often of a gelatinous consistency. Initially calves are bright and alert and have good appetites but if the diet is not corrected they become weak and emaciated.
Many infectious forms of diarrhoea are often complicated by poor quality feeds or insufficient nutritional intake.
When calves/lambs/kids start to graze they can also develop diarrhoea due to worm infection (see: link worms).
Another possible cause for diarrhoea can be plant poisoning (see: plant poisoning) and contaminated feed (especially Aflatoxin!).
Usually it is difficult to make a definite diagnosis based purely on the clinical signs. However, a presumptive diagnosis may be made based on the history, age of the calf, and symptoms. Faecal samples from both sick and healthy calves should be taken for submission to a laboratory, together with, if possible, a living sick animal.
Prevention and Control
The most important protection against diarrhoea for the young comes from the mothers colostrum,which protect the young during its first months of life. Colostrum given too late is a main cause of diarrhoea.
It is possible to identify the different diarrhoea agents responsible in a laboratory, but this may take too long because the disease develops too fast. Only some diarrhoea pathogens have specific treatments, for example Coccidia. Re-hydration treatment applies to all different forms of diarrhoea and must be started very early, when the calf is still able to stand and suckle.
Many pathogens of the intestine also produce toxins that can kill the animal fast. Charcoal powder absorbs the toxins and helps remove them from the body.
So first treatrment on observing a problem is rehydration liquids mixed with charcoal powder.
It is possible to identify the different diarrhoea agents responsible in a laboratory, but this may take too long because the disease develops too fast. Only some diarrhoea pathogens have specific treatments, for example Coccidia. Re-hydration treatment applies to all different forms of diarrhoea and must be started very early, when the calf is still able to stand and suckle.
Many pathogens of the intestine also produce toxins that can kill the animal fast. Charcoal powder absorbs the toxins and helps remove them from the body.
So first treatrment on observing a problem is rehydration liquids mixed with charcoal powder.
Certain broad principles apply to all herds.
- A new-born calf must drink at least 5% of its bodyweight of colostrum, preferably during the first 2 hours after birth, and certainly within the first 6 hours after birth. Adequate feeding of colostrum to calves at birth provides passive immunity to calves. A significant portion of both naturally sucking calves and handfed calves do not acquire adequate amounts of immunoglobulin because of delayed sucking or feeding, ingestion of an inadequate volume of colostrum, or ingestion of colostrum of inferior immunoglobulin concentration.
- Always Provide clean water to young calves/lambs/kids for drinking
- Vaccination of mother and calf against specific infections, such as E.coli can help to increase the resistance of the newborn.
- Clean calf pens regularly. Do not allow faeces to accumulate.
- Avoid over crowding of calves, and reduce the degree of exposure by isolating diseased animals, moving calving and calf rearing to a separate area and practising good hygiene.
- Find out which specific organism is causing the disease. This requires a laboratory test on a faecal sample or rectal swab handled by a skilled veterinarian, since some of these pathogens are harmful to humans. Where the pathogens are known, the right antibiotic, if indicated, can be given.
Treatment
The most important treatment measure regardless of the cause of diarrhoea is rehydration. Calves do not show signs of dehydration until they have lost at least 6% of their body weight. So do not wait! Calves still able to stand should be given oral electrolyte solution (rehydration fluid)that contains also Glucose to provide the calf with energy. You can also add honey instead of Glucose.
- Mix 5 tablespoons of sugar and 1 tablespoon of salt with 2 litres of clean water (boil water and let it cool down before mixing). Instead of 5 tablespoons sugar it is also very good to use 5 tablespoons of honey. A calf of 30kg needs minimum 3litres per day (minimum 1 litre for 10 kg of body weight per day). Feed the rehydration fluid in small portions at the rate of one and a half cup full at a time (equal to about 0.5litre). Kids and lambs need less of the fluid because they are much smaller (minimum 0.1litre per kg body weight per day).
- Rehydration fluid should be given for five days.
- In addition finely crushed charcoal (like powder) can be added to the rehydration fluid (2 handful of charcoal powder per litre, then passed through a sieve before giving it to the calf).
Milk may be withheld for first 24 hours but not for longer than 36 hours. So from the the second day on you can start giving small amounts of milk while still feeding rehydration fluid.
Calves that are recumbent and weak need both oral and intravenous electrolyte therapy for which the services of a veterinarian will be required.
Antibiotics are not required to treat diarrhoea caused by viruses, or protozoa such as cryptosporidia or coccidia. In cases of septicaemia due to E.coli or Salmonella antibiotic may be helpful (use injectable antibiotics).
Coccidiosis is easy to confirm in the laboratory and should be treated with specific anti-Coccidia drugs (Amprolium, also some sulphonamides given orally).
Calves that are recumbent and weak need both oral and intravenous electrolyte therapy for which the services of a veterinarian will be required.
Antibiotics are not required to treat diarrhoea caused by viruses, or protozoa such as cryptosporidia or coccidia. In cases of septicaemia due to E.coli or Salmonella antibiotic may be helpful (use injectable antibiotics).
Coccidiosis is easy to confirm in the laboratory and should be treated with specific anti-Coccidia drugs (Amprolium, also some sulphonamides given orally).
Enterotoxaemia is caused by the bacterium Clostridium perfringens, an organism which is widely distributed in the soil and in the gastrointestinal tract of animals. It is characterized by the ability to produce potent exotoxins (poisons). The bacteria are also capable of forming spores which survive for long periods in soil. Five types have been identified, the most important of which are A, B, C and D.
The spores of Clostridium perfringens Types B, C and D are found in soil and faeces of normal animals in areas where disease is prevalent as well as in the intestinal contents of infected sheep. Their presence in the intestinal tract of normal animals is important because they are able to form the focus for a fatal infection as and when conditions alter to allow their rapid multiplication.
The organism multiplies extremely rapidly in the presence of high levels of carbohydrate when oxygen tension is low. Thus, in cases of Lamb Dysentery, disease is most prevalent in lambs which ingest large quantities of milk. So heavily-milking breeds are more susceptible than lighter-milking breeds. A similar situation exists with Pulpy Kidney Disease, when a change of diet from one consisting mostly of roughage to one predominating in grain, allows starch granules to move into the duodenum, where they form an ideal medium for the multiplication of the bacteria, which produce toxin (poison).
Type A
This occurs as part of the normal, intestinal microflora of animals, and produces the lethal and necrotizing alpha toxin, causing necrotic enteritis in poultry and dogs, colitis in horses and diarrhoea in pigs.
The disease is characterized by a necrotic enteritis in which there is massive destruction of the villae (small finger-like projections in the gut which increase surface area and thereby improve food absorbtion), and coagulation necrosis (death of tissue) of the small intestine. In dogs there may be a haemorrhagic (bloody)diarrhoea.
Types B and C (Dysentery)
These types cause severe enteritis (stomach infection), dysentery (very severe diarrhea, often with blood and mucous), toxaemia (blood poisoning) and high mortality in young lambs, calves, pigs and foals.
Types B and C both produce the highly necrotizing and lethal beta toxin, which is responsible for severe intestinal damage. Adult cattle, sheep and goats can be affected by enterotoxaemia caused by Type C.
Lamb Dysentery occurs in lambs up to three weeks of age and is caused by Type B.
Calf Enterotoxaemia is caused by Types B and C in well fed calves up to one month of age.
Pig Enterotoxaemia occurs during the first few days of life and is caused by Type C.
Foal Enterotoxaemia occurs during the first week of life and is caused by Type B.
Struck is caused by Type C in adult sheep, while Goat Enterotoxaemia in adult goats is also caused by Type C.
Signs of Enteroxamia (Dysentery)
Lamb dysentery is an acute disease of lambs less than three weeks old. Many die before symptoms are seen. Others stop suckling, become listless, have a foetid (foul smelling), blood-tinged diarrhoea and die within a few days.
In calves there is acute diarrhoea, dysentery, abdominal pain and convulsions. Death may occur within a few hours, but less severe cases may survive for a few days and occasionally recovery may occur.
Most affected piglets die within a few hours with diarrhoea and dysentery.
In foals there is acute dysentery, toxaemia and rapid death.
Struck is characterized by sudden death in adult sheep.
Diagnosis
Post mortem findings reveal in all cases a haemorrhagic (bloody) enteritis (Stomach infection) with ulceration of the mucosa. Smears of the gut contents reveal large numbers of gram positive rod-shaped bacteria, while filtrates will reveal and identify the toxin.
Control and Prevention
Because the disease is so severe, treatment is usually ineffective. Oral administration of antibiotics may be helpful in some cases.
The disease in lambs is best controlled by vaccination of the pregnant dam during the last third of pregnancy, initially 2 vaccinations one month apart and annually thereafter.
When outbreaks occur in newborn animals from unvaccinated dams, antiserum, if available, should be administered immediately after birth.
The disease in lambs is best controlled by vaccination of the pregnant dam during the last third of pregnancy, initially 2 vaccinations one month apart and annually thereafter.
When outbreaks occur in newborn animals from unvaccinated dams, antiserum, if available, should be administered immediately after birth.
Type D (Pulpy Kidney Disease)
This type causes Pulpy Kidney Disease of sheep.
It occurs world wide and may occur in animals of any age, but occurs most commonly in 3 ? 12 week old lambs and in fattening lambs 6 - 12 months old. Single lambs are more susceptible than twins. Morbidity seldom exceeds 10% but mortality is usually 100%.
It is caused by the rapid multiplication of the organism in the small intestine and the subsequent absorption of the epsilon toxin, which is produced by the organism in the form of a non-toxic prototoxin and is converted to a lethal toxin by the action of trypsin.
The toxin increases the permeability (ability to pass through) of the intestinal mucosa to this and other toxins, thus facilitating its own absorption. The first effect of the toxin is to cause a profuse (heavy), mucoid (slimy) diarrhoea and then to produce a stimulation and then a depression of the central nervous system.
Lambs on lush grazing or being fed grain in feedlots, are particularly at risk.
Signs of Pulpy Kidney disease
Pulpy Kidney Disease is peracute (very severe) and of short duration, with most cases being found dead. Those that are observed before death show hyperaesthesia (excessive reaction to being touched and other stimuli), staggering progressing to lying down, with its head twisted back over the back, intermittent convulsions, occasional diarrhoea and death. Affected animals do not recover.
Diagnosis
At post mortem
- the animal is usually in good condition
- there is an excess of straw-coloured fluid around the heart,
- haemorrhages (bleedings) are present in the heart.
- The liver is swollen and friable and some congestion of the intestinal mucosa may be present.
- The appearances of the kidneys can be quite characteristic. In a fresh carcass they appear swollen and pale, but after a few hours they soften more rapidly than normal, giving the disease its name.
In lambs the circumstances of sudden convulsive death in the best conditioned lambs, together with the post mortem findings are usually sufficient to be diagnostic.
Smears of intestinal contents may reveal many short, thick gram positive rods. Confirmation requires the demonstration of epsilon toxin in the small intestinal fluid. Fluid, not ingesta, should be collected in a sterile vial, within a few hours after death and sent refrigerated to the lab for toxin identification. Chloroform added at 1 drop for each 10mls of intestinal fluid will stabilize any toxin present.
Control and Prevention There are two main control measures available:
1. reduction in the food intake. Moving lambs from a lush pasture to a poorer one may help to minimize losses, and similarly avoidance of any sudden changes in diet which are likely to result in acidosis and promote conditions favourable to multiplication of the organism and production of toxin.
2. Vaccination: Ewe immunization is probably the most satisfactory method of control. Breeding ewes should be given 2 injections of Type D Toxoid in their first year and 1 injection 4 - 6 weeks before lambing each year thereafter.
Lambs should receive their first vaccination dose when 8 - 12 weeks old and a second dose 4 - 6 weeks later.
Polyvalent vaccines protecting against other clostridial diseases such as Blackquarter, and Tetanus, frequently incorporate components protection against Lamb Dysentery and Pulpy Kidney Disease, and the manufacturer?s instructions should be closely adhered to.
|
Scientific name:
Aphtae epizooticae
Local names
Luo: olawo, achany / Maragoli: azuya / Gikuyu: muguruma / Gabbra: oyale / Kamba:muthingithu / Kipsigis:ngworek / Maasai: Olkuluk, loirobi, olguluk / Samburu: ikulup / Somali: dila, labeb, abeb, abeeb / Swahili: ugonjwa wa miguu na midomo / Turkana:lojaala, ebaibai, lokulup / Luidakho: man'gwali / Luvugusu: gamalenge / Nandi: maikutiet
Common names:
afthosa, aphthos fever, fievre aphteuse (French) fiebre aftosa (Spanish)
Description
Specific management disease
Introduction
Foot and mouth disease is a highly contagious viral infectious disease of cattle, sheep, goats and pigs. It can also affect wild animals, especially buffalo, which act as significant hosts, and in which the disease is generally much milder than in cattle. It is caused by seven serotypes of Foot and Mouth disease virus namely: A, O, C, SAT 1, SAT 2, SAT 3 and ASIA 1.
Mode of spread The virus can be harboured for periods in the nose and throat of wild animals.
The importance of the disease in small stock such as sheep and goats is largely as carriers of the disease to cattle; but in Kenya it has been shown that goats are infrequent carriers and sheep not at all. The disease is enzootic in many parts of the world .
FMD is mainly transmitted through inhalation or ingestion of the virus from contaminated feeds and direct contact with infected animals. The incubation period is on average 3 to 8 days after the animals are infected with the virus. Infected animals will then discharge the virus to materials they are in contact with or directly to other animals, thereby infecting them. This can be through the saliva, rupture of vesicles and blisters on the tongue and feet, discharges from the nose, and through coughs.
Meat, milk and semen from infected animals can spread infection.
Humans can also transfer infection to other animals through movement of people and vehicles from infected premises to susceptible areas. People working with infected cattle can harbour the virus in their nasal mucosa for up to 28 hours. Ticks also spread infection.
Windborne spread can be important under certain conditions as can spread by flocks of birds.
The important thing to remember is that this is one of the most contagious diseases known, and to act accordingly by taking every possible measure to prevent the entry of infection.
|
|
Signs of foot and mouth disease
- Severe lameness, due to the presence of blisters and vesicles between the toes, which then rupture and become secondarily infected
- The animals develop a high fever, become weak and dejected, and there is a rapid loss of condition. Mortality in calves is high
- Cattle stop eating due to the pain arising from the lesions in the mouth
- There is a drastic drop in milk production
- The coat becomes rough and there are blisters and vesicles inside the mouth especially on the tongue. There is profuse salivation with long ropey strings of saliva, and a characteristic smacking of the lips
- Blisters also form above and between the claws, and some blisters appear on the teats.
- Abortion is common
- Most animals recover but there is a frequent chronic and sometimes permanent loss of condition.
- In some instances, heart failure may occur causing sudden death
- Any combination of salivation and lameness with blisters and vesicles in the mouth must always be regarded as being Foot and Mouth Disease until proved otherwise
- Sheep and goat suffer a much milder disease than cattle
- Also pigs can be affected by Foot and Mouth disease:
 |
| Typical posture of pigs with painful blisters on the feet |
| © USDA |
Diagnosis
- Clinical signs and history
- Samples of vesicular fluids and epithelium can be sent to the lab for confirmation and sero typing at FMD Research Institute at Embakasi in Nairobi, Kenya.
- Differentiate diagnosis with Foot rot for leg and foot lesions. The disease can also be confused with Bluetongue.
Diseases with similar symptoms
- Leg and feet lesion: see Foot rot
- Mouth lesions: see Rinderpest
- In sheep can be confused with Bluetongue
Prevention - Control - Treatment
Prevention and Control
- Report occurrence immediately so as to invoke quarantine after the disease is confirmed by the veterinary authorities. Such quarantines should be lifted only by the authorities, usually 6 weeks after the last recorded case.
- Disinfect premises and motor vehicle tyres with suitable disinfectant to prevent further infections.
- Vaccinate regularly. This should be done after determining the strain of the virus in order to give the correct sero type vaccine. Usually a multivalent vaccine is administered every 6 months as preventive measure. Outbreaks have occurred following vaccination and have been attributed to the production of carrier animals.
- Strict adherence to sanitary measures e.g. destruction of feed and beddings of infected animals.
Recommended treatment
There is no medical treatment for Foot and Mouth Disease. However, you can help the animals to recover:
- Shade them from the sun and give them plenty of water
- Give them soft feed such as green, soft, lush grass, which is better than hay as the blisters make it painful for the animals to eat. The addition of molasses is advised to give the animals energy.
- Use Magadi soda for foot baths and wound treatment.
- Give antibiotics by intramuscular injection to prevent secondary infection of the blisters.
| WARNING: Do not give antibiotics by mouth to adult cattle, camels, sheep and goats. It makes these animals sick by destroying essential bacteria in their rumens that are there as a vital part of the digestive process. |
Common traditional practices
Some of these are sensible and useful. Feeding of easily digested energy feeds are very beneficial as are disinfection of wounds with Magadi soda.
- Kipsigis: Mix 10kg of maize flour in 10 litres of water. Add 2kg of pounded finger millet. Allow to ferment for 3 days. Give an infected animal 4 litres of this brew to drink. Treatment for hooves: Spread 5kg of ash or 5kg of Magadi soda mixed with 5kg of ash in the morning and in the evening, at the entrance of the boma so the cattle must walk through it on the way to graze and when they return.
- Luo: Pound half a handful of fresh olulusia (Vernonia amygdalina) roots. Mix with 4kg of finger millet flour and 5 litres of water. Sieve and drench adult cattle with 2 litres (1 litre for calves, goats and sheep) twice a day until recovery.
- Turkana: Mix 500g of Magadi soda in 5 litres of water. Use the mixture to treat wounds in the mouth and externally on feet and teats. Repeat twice a day until recovery.
Local names:
Luo: achany, abok / Borana & Gabbra: okol, bargao / Kipsigis: moeet / Gikuyu: rugumo / Maasai: Alelei, en jalan / Maragoli: bulwaye vwe tsimbagayu / Samburu: ngojini, namurie / Somali: raaf-dila, rafqarir, gumeed, rafdilnac, rafjac, bog, boog / Turkana: ekichodinu, ebaibai /
Luo: achany, abok / Borana & Gabbra: okol, bargao / Kipsigis: moeet / Gikuyu: rugumo / Maasai: Alelei, en jalan / Maragoli: bulwaye vwe tsimbagayu / Samburu: ngojini, namurie / Somali: raaf-dila, rafqarir, gumeed, rafdilnac, rafjac, bog, boog / Turkana: ekichodinu, ebaibai /
Common names:
foul-in-the-foot, pietin, pietur (French), pedero (Spanish)
Introduction
Following periods of prolonged rain, outbreaks of foot rot appear in cattle, sheep and goats, even those kept under extensive production systems. Humid, warm conditions favour the organisms responsible. Foot rot can be a major disease problem under intensive dairy production systems, especially when zero-grazing is practised.
Other factors such as breed and housing are known to influence the occurrence and severity of the disease. Under intensive systems where exotic breeds are kept, the disease occurrence is more severe than in extensive systems where most indigenous breeds are normally kept.
The disease has negative economic consequences to the farmer because it hinders the animal from feeding at the time when there is plenty of good feed. Serious foot problems reduce the productive life-span of the dairy cow, which has to be culled too early.
|
|
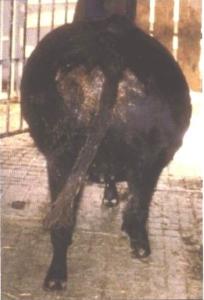
Foot Rot in Cattle
In cattle different bacteria are involved in foot rot, the most important one being Fusobacterium. These bacteria are also present in faeces, which explains why the disease is more common in dirty environment and is also difficult to control.
|
Causes
The bacteria causing foot rot are normal residents of the environment of cattle but cannot penetrate healthy skin. Any injury to the foot and especially to the skin between the toes provides an entry for foot rot bacteria and allows these pathogens to infect the skin and the tissue underneath the skin. Injury occurs easier and more frequently in skin that has been softened by constant exposure to water, faeces and urine.
The animals contract the disease when they walk in wet, muddy places which have been contaminated by animals with foot rot.
Adult cattle are more commonly affected than younger animals and local breeds of cattle appear to more resistant than those of European breeds.
Signs of Foot Rot
|
|
Prevention
- Keep the ground clean and dry, especially in zero grazing(!), you can use saw dust to keep the surface dry
- If you have concrete surface make sure the surface is very even and smooth - uneven and rough concrete surface causes injury to the hooves
- Frequently clean, sweep and scrape hard surfaces free of manure; remove dung and mud from the boma regularly
- Drain areas around drinking troughs, gateways and frequented tracks.
- Trim hooves regularly, any overgrowth should be cut off when you see it, always keep the hooves in normal shape
- Cows with soft hooves are more likely to suffer from foot rot, do not buy or keep offspring from such cows
Treatment
Treatment must begin as soon as possible!
- If there is already a large lesion, wash the foot especially the skin between the claws with hot water- as hot as you can put your hand in; then apply an antiseptic solution like dettol or similar; cut away or trim any decayed part of the hoof to remove the infection that is underneath it, remove all dead tissue using a clean pen-knife; treat surface with Hydrogen Peroxide 3% and cover with a wound powder/ointment (e.g. copper sulphate in the form of a blue paste); make sure the animal is kept on dry clean surface
Caution: when trimming the hooves inexperienced people may cut too deep causing extra injury - it is very good to watch an experienced stockman trimming hooves and learn from him
- After operating on the foot supportive treatment with antibiotics is necessary: good results are obtained with Procaine-Penicillin or Penicillin-Streptomycin IM for 3 days at double the normally recommended dose; long-acting Oxytetracycline also gives good results as does a three day course of Trimethroprim/Sulphadaizine IM
Common traditional practices
- Somali: Wash the foot with very salty water repeatedly until the animal recovers
|
Foot Rot in Sheep/Goats
In sheep/goats Foot Rot is a serious herd problem that can affect many sheep/goats and spread rapidly through the entire flock. In most cases more than one foot is affected.
Causes In Foot Rot two organisms are required to start the infection - Fusobacterium necrophorum and Dichelobacter nodosus. Fusobacterium lives in the sheep's guts and environment and can also affect cattle. Fusobacterium alone cannot cause Foot Rot. Dichelobacter lives only in the affected hooves of carrier sheep/goats and is the main cause for foot rot. During rainy Dichelobacter can survive for maximum two weeks on soil or pasture and infect more sheep/goats. Foot Rot is transmitted via the contaminated environment. If healthy sheep/goats share pasture, watering points and/or the boma with Foot Rot infected sheep/goats they pick up the infection while passing through contaminated areas
Signs
|
|
|
Prevention & Control
|
|
Treatment
The success of any treatment is much greater if the sheep are kept in a completely dry environment after treatment. The feet of treated sheep should be examined every 1-2 weeks to identify those needing further treatment.
Diseases with similar signs/symptoms
|
|
Local names:
Borana: quando / Samburu: nalngiarrngarri / Somalia: kharar / Turkana: angaare
Borana: quando / Samburu: nalngiarrngarri / Somalia: kharar / Turkana: angaare
Description:
Respiratory disease
Introduction
Haemorrhagic Septicaemia also sometimes called "shipping fever" is an acute bacterial disease of cattle and water buffaloes and pigs. It is caused by Pasteurella multocida serotypes B2 in Asia and E2 in Africa.
Also Fowl Cholera is caused by Pasteurella sp.
Outbreaks of acute pasteurellosis caused by other serotypes of P. multocida or by P. haemolytica should not be called Haemorrhagic Septicaemia, even though septicaemia may be a feature.
The disease is endemic (insert dictionary) in south and east Asia. Occasionally outbreaks occur in Africa, southern Europe and the Near East.
Mode of spread
Only water buffalo and cattle are regularly affected. Stress factors, coupled perhaps with viral or other infections, weaken the animals' defences and predispose them to the disease. The disease in Africa may suddenly appear and then may not reappear for many years. The worst outbreaks occur during the rainy season.
- Transporting and herding animals may trigger an outbreak.
- Spread within a group usually occurs at night when animals are enclosed, and between groups via communal watering points.
- In areas where the disease is prevalent, small numbers of healthy animals - cattle and water buffalo - carry the bacteria in the nasopharynx (the area of the upper throat that lies behind the nose) or tonsils and act as reservoirs of infection. Bacteria are then spread through the air.
- During an outbreak sick animals excrete large numbers of bacteria in runny noses, saliva and faeces.
- For several weeks after an outbreak 20 - 50% of animals carry the organism and are capable of infecting susceptible in-contact animals.
- Indirect transmission can also occur.
- The causal bacteria can survive for several hours in moist conditions, but die rapidly if exposed to sunlight or thorough drying
|
Signs of Haemorrhagic Septicaemia
In areas where the disease is prevalent, animals over 1 year old have often acquired immunity from previous outbreaks, therefore disease is more common in young stock. Outside such areas, clinical cases are seen in all age groups.
|
|
Diagnosis
Rapid course of illness, high herd incidence, weather conditions, fever, typical throat swellings, coupled with the characteristic post mortem findings, are suggestive of Haemorrhagic Septicaemia.
Anthrax, gas gangrene caused by clostridial bacteria, certain snake bites, and pneumonic pasteurellosis should be considered, as these can occasionally give rise to similar swellings.
- Post-mortem reveals extensive oedema of the head, throat and brisket. The fluid is straw coloured and infiltration may extend from the subcutaneous tissue into the muscle.
- Numerous small haemorrhages are found throughout the carcass.
- Blood-tinged fluid may be found within the pericardial sac and in the chest and abdominal cavities.
- The pharyngeal and cervical lymph nodes are swollen and frequently contain small haemorrhages.
- In those animals which have survived for several days pneumonia with thickening of the interlobular septae may be seen, but well- established bronchopneumonia is more likely to be caused by other serotypes of P. multocida or P. haemolytica than in true Haemorrhagic Septicaemia.
- When calves are affected haemorrhagic gastroenteritis may be seen.
To confirm the diagnosis, a veterinary surgeon will take samples of tissue from blood, lung, liver and spleen and send these to a laboratory to determine the organism that has caused the disease. If the animal has been dead for longer than 8 hours, the vet will send a long bone.
Diseases with similar symptoms
- Swollen lymph nodes, fever and froth discharge from the mouth: See ECF and MCF (under construction)
- Anthrax, Salmonellosis (under construction), Rinderpest - see below
Prevention - Control - Treatment
Treatment
To be of value, treatment must be started early; but because of the rapid course of the disease, this is often not practicable. Treatment is of little value once animals appear shocked, and may instead cause a deadly crisis by causing death of organisms and the release of toxins produced by the bacteria.
Various sulphonamides, tetracylclines, penicillin and chloramphenicol are effective if administered in the very early stages.
Prevention
- The principal means of prevention is by vaccination, which in areas where the disease is prevalent, should be carried out on an annual basis.
- Where the disease is not prevalent, the cost of regular vaccination may not be justified, but when an outbreak occurs, vaccination should be considered in order to control the spread of infection.
- Herd quarantine, the segregation of sick animals from healthy ones, and routine disinfection all help to slow the spread of disease between and within herds.
- In previously infected herds, natural immunity exists and occurrence rates and death rates are substantially lower than in herds not previously infected. Immune animals, however, can carry and transmit infection.
Local names:
Luo: Tuo thuno / Embu: yele / Borana & Gabbra:hiha goru, butha / Kamba: Uwau wa nondo, mukamo / Kipsigis: miatapkinai / Maragoli:lifuuti / Somali: candho-barar, canda-barar, carar, galleh, goof / Turkana: loebeta / Kikuyu: Murimu wa nyondo, kuruara mukamo / Maasai: Enkeeya Ollki / Kiswahili: matiti
Luo: Tuo thuno / Embu: yele / Borana & Gabbra:hiha goru, butha / Kamba: Uwau wa nondo, mukamo / Kipsigis: miatapkinai / Maragoli:lifuuti / Somali: candho-barar, canda-barar, carar, galleh, goof / Turkana: loebeta / Kikuyu: Murimu wa nyondo, kuruara mukamo / Maasai: Enkeeya Ollki / Kiswahili: matiti
Common names:
mammitis, mammite (French), inflammation de la ubres (Spanish)
mammitis, mammite (French), inflammation de la ubres (Spanish)
Description:
Management disease
Management disease
|
Introduction
Mastitis is inflammation of the udder, the udder is also called mammary gland. Mastitis is mainly a problem in dairy cows but sometimes acute mastitis can also be a problem in dairy goats. However mastitis can affect all milk producing animals as well as humans.
Most mastitis cases result in relatively mild or undetectable inflammation of the udder; called subclinical mastitis. This form of mastitis can persist for the whole life of the cow. The milk gland tissue first hardens and is then slowly destroyed, which can take several lactations until the udder or quarter stops to produce milk at all. The persistent infection in the udder affects the quantity and the quality of the secreted milk. Subclinical mastitis can reduce the milk yield by 40% ! It also spoils the milk quality resulting in rejection of the milk by milk collectors and milk consumers. - All dairy herds have cows with Sub-clinical Mastitis. The percentage of cows infected with subclinical mastitis can be as high as 755.
Seldom occurring but more severe cases of mastitis lead to painful swelling of the affected quarter, abnormal milk, total loss of milk yield or even more severe illness and even death; this form is called clinical mastitis.
|
|
Mastitis is caused by different bacteria (especially Streptococci, Staphylococci and bacteria originating from the gut, such as E.coli) and is contagious. The bacteria invade the udder through the teat canal.
The most important reservoir of mastitis bacteria is the infected udder. Transmission occurs at milking via the milkers' hands or via the milking equipment.
The most important reservoir of mastitis bacteria is the infected udder. Transmission occurs at milking via the milkers' hands or via the milking equipment.
The infection can spread from one teat/quarter to another and from one animal to another:
- Via the hands of the person milking
- Through milking bucket and cloth
- Via flies
- Via the liners of the milking cup (if milking machine is used)
- Via the mouth of the suckling young (esp. kids)
- Through environmental contamination of the stable or the boma (wet and dirty beddings)
- Through contaminated water
- Via contaminated teat dips
- Via intra-mammary infusions
- Teat skin lesions and wounds
- Heifers can become infected with mastitis prior to calving, especially if there a lot of flies.
The risk of a cow being affected by mastitis increases with the level of milk production.
Factors that increase the risk of mastitis are:
- Early lactation, when animals give a lot of milk
- High milk yield
- Abnormal teats, the shape of the teat play an important part, as do the presence of wounds on the skin of the teat, especially if they are near the opening
- Lack of hygiene in the milking parlor and during milking
- Adult cattle are most at risk than young ones and can be infected when lactating or during dry period
Pigs sometimes get mastitis immediately after giving birth when the piglets are very young.
Trauma and injury during milking or during fighting between cattle can damage the teat !!!
Mycoplasma are special bacteria, which may spread from cow to cow through the air. They infect the body of the animal and then invade the udder via the blood. This is a very specific infection which infects all cattle, causes mastitis, respiratory disease, abortions and makes the whole herd unproductive.
Sheep and goats can also get a very severe form of mastitis called Contagious Agalactia, caused by another type of mycoplasma, which has similar devastating effect on the goat herd (mastitis, arthritis, abortion, septicemia) as the other mycoplasma in cattle.
Sheep and goats can also get a very severe form of mastitis called Contagious Agalactia, caused by another type of mycoplasma, which has similar devastating effect on the goat herd (mastitis, arthritis, abortion, septicemia) as the other mycoplasma in cattle.
Signs of Mastitis
Sub-clinical Mastitis ( "invisible mastitis" because it has almost no visible signs)
- This form of mastitis can persist for the entire lactation and even for the entire life of the cow. Persistent infection of the udder can reduce the milk yield by up to 40%!
- Sometimes small changes in the milk can be detected, small particles are visible in the milk using a strip cup.
- Detection is possible by laboratory examination of the milk to identify the pathogen and also identify the best drug for treatment. Because this mastitis persist for a long time information from the lab can be very useful for the treatment.
- The most efficient way to detect sub-clinical Mastitis is by testing the milk using the California Mastitis Test (CMT), which can be done on the farm. After mixing equal volumes of milk and CMT fluid in the paddle the milk from infected quarters will show higher viscosity (be thicker) than the milk from normal quarters. Testing must be done before milking.
Mild Clinical Mastitis
In dairy cows this form of severe mastitis is caused by fecal bacteria from the gut (e.g. E. coli). There is severe illness affecting the entire body, loss of appetite, depression, toxemia (blood poisoning), septicemia (bacteria in the blood). The cow may not be able to stand up and death is possible within a few days. - A similar mastitis in dairy goats can be caused by Staphylococcus (a bacterium normally causing wound infections and pus).
|
|
|
Mastitis during the dry period can be especially serious, sometimes leading to complete loss of udder tissue and abscess formation. There is also a form of mastitis which starts during dry period but becomes visible immediately after calving. The milk appears like pus, looks green or yellow-green and have a foul smell (this can also happen in first calving heifers) and cause blockage of the teat canal |
Prevention - Treatment
Subclinical mastitis is difficult and expensive to treat. Infections often persist despite treatment. Also wrong application of intra-mammary tubes can introduce more dangerous pathogens into the udder than the ones already present. For example fungi can be introduced into the udder by dirty or repeatedly used intra-mammary tubes and can cause life threatening mastitis which is impossible to treat. Intra-mammary tubes must be stored in a very clean place; once the cap has been removed from the tube it must be used immediately. Contents of one tube treat only one teat - always use one complete intra-mammary tube for one teat, don't split the same tube between two teats.
|
|
||||||
|
|
The most important is to prevent infection of the udder with mastitis bacteria. This can be done by applying strict milking hygiene:
- Milk in a clean environment (no flies!); areas around dairy shed must be dry and free of mud and standing water
- Where machine milking is practiced a footbath with disinfectant should always be provided; teat cup linings can cause damage to the teats and must be changed frequently; vacuum of the milking machine must be checked and the machine must be serviced regularly
- Milk room hygiene including washing of containers and equipment must be continuous
- Use very clean milking equipment
- Wash and dry the teat before milking; it is simple and safe to dry the teats using tissue paper (toilet roll) for cleaning the teats before milking; udder clothes must be disinfected or boiled and allowed to dry in between milking times - otherwise the cloth becomes a source of infection
- Wash hands with soap before milking; clean water mixed with a disinfectant should always be available in the dairy (disinfecting dirt does not work, you have to remove the dirt by washing with soap first, then disinfect the skin)
- Wash teats before milking
- Use milking salve to protect the teat skin; hand milking must be gentle and never rough; treat all wounds of the teat or of the udder skin with iodine or healing oil as long as the wound is still fresh
- Use the strip cup before each and every milking; first milk squeezed out from each quarter and used to test for mastitis should not be dropped on the floor but should be collected in a separate container with a dairy disinfectant
- Test your cows with CMT regularly
- Use iodine teat dip (contains 1% iodophor or 4% hypochlorite) after milking and change teat dip regularly (the teat dip acts as a barrier and prevents bacteria from entering the teat canal); teat cup must be cleaned and disinfected in between milking times
- Milk cows with mastitis last; always milk CMT-negative udders and young cows first, because their udder are less likely to be infected; this prevents spread of mastitis from one cow to another
- For high yielding cows during early lactation milking three times a day is recommended
- Old cows with chronic mastitis and abnormal teats and cows with persistent mastitis should not be treated but culled
Dry Cow Therapy is more efficient in eliminating subclinical mastitis than treatment during lactation because in the dry period the drug can act for much longer inside the udder. Consult your veterinarian.
How to apply intra-mammary tubes (example: for dry cow therapy) correctly into the teat.
Step 1: Milk the udder until it is completely empty
Step 2: Clean and dry the end of the teat
Step 3: Apply disinfectant to the tip of the teat
Step 4: Put the nozzle of the tube into the teat and squeeze the content up into the teat
Step 5: Massage the teat upward
Step 2: Clean and dry the end of the teat
Step 3: Apply disinfectant to the tip of the teat
Step 4: Put the nozzle of the tube into the teat and squeeze the content up into the teat
Step 5: Massage the teat upward
After using intra-mammary tubes the milk contains antibiotics and must not be used for human consumption. Observe the withdrawal period which is given by the manufacturer on the intra-mammary tubes.
|
|
The most damaging and persistent pathogen causing subclinical mastitis is Streptococcus agalactiae. It is also the only mastitis pathogen that can be eradicated from a herd. If a laboratory has identified this pathogen in your milk you should consult a veterinarian to make a control plan.
Acute or Severe Clinical Mastitis
Treatment of acute severe mastitis is a race against time. Urgent treatment is required and the services of a veterinarian should be sought immediately. Acute or severe mastitis requires intensive intramuscular and intravenous treatment: antibiotics combined with supportive treatments in the form of fluids (Glucose, electrolytes) and anti-inflammatory drugs are required to save not only the affected quarter but also the cow?s life. While you wait for the veterinarian to arrive empty the affected quarter repeatedly to remove as much liquid, which is full of toxin, as possible. You can also try to cool the affected quarter to reduce the swelling.
Local names:
Kikuyu: Murimu wa iria
Scientific name: Parturient paresis
Description: Specific diseases
Scientific name: Parturient paresis
Description: Specific diseases
Introduction
Milk fever is a condition of mature dairy cows that occurs a few days before, but mostly just after calving. It is common in imported high yielding dairy cows, especially Friesian or Channel Island breeds such as Jersey or Guernsey. Milk fever does not occur in indigenous cows.
Milk fever is caused by low calcium levels in the body due to the sudden onset of lactation at calving. The nutritional status of the cow in the dry period is known to influence the risk of the disease. Diets low in dry matter such as lush pastures and diets with high calcium during dry period can predispose the cow to milk fever. Low magnesium in the diet hinders absorption of calcium and hence predisposes the cow to milk fever.
The disease is more risky in cows after third calving and is rare in calving heifers.
Signs of Milk fever
- The first sign of the disease is loss of appetite, followed by a slight drop in temperature.
- The affected animal become uncoordinated, falls over and remains seated with its head resting on its shoulder.
- Dull eyes and shivering, constipation is a common feature and sometimes a wobbly gait is seen.
- If not treated immediately, the animal may go into coma and die within a day after the first signs. Since the rumen stops functioning, bloat becomes a complication and may cause death.
Diagnosis
- Based on history, recent calving or near calving
- Clinical signs and response to calcium treatment
- Blood samples can be taken to the laboratory for calcium and phosphate levels
Diseases with similar symptoms
- Differentiate diagnosis with Ephemeral Fever where the cow goes recumbent
Prevention - Control - Treatment
Prevention and Control
- Feed the cow with the correct levels of nutrients from late pregnancy to peak lactation
- Feed diets with the right dry matter content such as offering additional hay in combination with lush pasture.
- Feed balanced mineral supplement which appreciates the inter-relationship between calcium and magnesium
- Right after successful calving give high yielding cows a handful of agricultural lime mixed with first feed. This will assist the cow in summoning enough calcium to produce milk.
- Let the calf suckle for the first 3-4 days with no extra milking. This will allow the cow to adjust gradually to produce milk. The first colostrum is not usually marketable anyway.
Recommended treatment
- If the cow is found to be lying on her side she should be immediately propped on to her chest, otherwise she is liable to get bloat or inhale stomach content with the attendant risk of developing aspiration pneumonia. DO NOT use rocks or boulders to prop!
- Slow intravenous infusion 400ml of 20% calcium borogluconate should be administered as soon as is possible. If this is difficult then give the same volume by subcutaneous ( For instructions see here: Vaccination) injection. Give in several sites and massage the sites of injection to disperse the solution.
- Response to treatment is seen by the cow belching, snapping and opening her eyelids, breathing deeply, passing dung and sitting up.
- Even if the cow appears to be unconscious give intravenous calcium. Even cases which look hopeless can recover.
- The calf should be removed and the cow not milked for 24 hours. On day two milk half the estimated volume from each quarter and feed this to the calf. On day three milk normally. If the calf is allowed unrestrained access to the cow or if unrestrained milking is carried out the cow may well go down again.
- Get a flutter valve and have it clean and ready for use. There is nothing more frustrating than trying to give 400ml calcium by intravenous injection with a 20ml syringe and it is guaranteed to damage the jugular vein.
Introduction
Peste des Petits Ruminants, otherwise known as Goat Plague or Pseudo-rinderpest, is an acute or subacute viral disease of goats and sheep characterized by fever, erosions and inflammation in the mouth, lips and tongue, gastroenteritis, pneumonia and death.
Goats are primarily affected, sheep less so and cattle are only sub-clinically affected. Humans are not at risk.
This is a disease which occurs mainly in the Sahel region of Africa, that area to the south of the Sahara; and the Middle East, to which it was introduced via large importations of goats and sheep from Africa.
A recent outbreak in north-west Kenya , entering via the Sudan , devastated many flocks of goats and sheep, which, not having encountered the disease before, suffered very high mortality.
Cause
The virus responsible is a member of the Morbillivirus genus of the Paramyxoviridae family. It shares antigens with other members of the genus. The virus of Peste des Petits Ruminants and that of Rinderpest partially cross protect. As Rinderpest has now been eradicated this fact is now of academic interest only.
Nomadic goats and sheep in the Sahel have a high innate resistance to PPR and usually undergo subacute reactions.
Mode of Spread
This is by close contact. Confinement favours outbreaks.
Secretions and excretions from sick animals are the sources of infection. New infections are initiated when the virus is inhaled by in-contact goats or sheep. The virus enters the new host through the cells of the upper respiratory tract and the conjunctivae.
Signs of PPR
1. Mortality in goats apart from the nomadic Sahel goat ranges from 77% to 90% and death usually occurs within a week of the onset of the disease.
2. An incubation period of 2-6 days is followed, in the acute form, by a sudden rise in body temperature to 40 - 41.3 degrees C.
3. Affected animals appear ill and restless, have a dull coat, dry muzzle, congested mucous membranes and a depressed appetite.
4. There is a clear nasal discharge which soon becomes filled with pus with an unpleasant smell. There may be sneezing.
5. The discharge from the nose and eyes encrusts the nose and matts the eyelids.
6. Severe destructive inflammation affects the lower lip and gums and the tissues where the lower front teeth are inserted into the gum are also similarly severely affected.
7. In more severe cases it may involve the dental pad, palate, cheeks and their papillae and the tongue.
8. There is intense depression and diarrhoea may be very heavy.
9. There is dehydration, hypothermia, followed by death, usually after 5 - 10 days.
10. Bronchopneumonia (inflammation of the lungs. Lungs develop redness, contain fluids, become heavy, may sink in water - general change in color) with coughing may develop in the latter stages of the disease.
The disease is less severe in sheep and sub-acute reactions are more common than in goats, manifested by nasal catarrh, low grade fever, recurring crops of mucosal erosions and intermittent diarrhoea. Most recover after a course of 10 - 14 days.
PPR may affect the immune system of the animals so that more complications arise. The most common activated complication is pasteurella pneumonia, but other latent infections may also be activated. Orf lesions of the lip, for example, commonly develop in surviving goats.
Diagnosis
The following post-mortem findings in goats and sheep possessing low natural resistance should point the way towards a diagnosis, with confirmation supported by the detection of specific antibodies in lymph nodes and tonsils and the isolation and identification of the causal virus by in cultured blood samples.
- The carcase is dehydrated and soiled with foetid, fluid faeces.
- Muco-purulent discharges encrust the nose and eyes.
- Necrotic lesions are seen inside the lower lip and on the adjacent gum, the inside of the cheeks and on the lower surface of the tongue. The erosions are shallow, with a red, raw base, which later becomes a pinkish white with a sharp edge.
- Severe lesions are frequently seen in the 4th stomach and in the large intestine.
- A prominent post mortem finding is a purulent bronchopneumonia masking an underlying primary viral infection, manifested as areas of level red consolidation.
Diseases with similar symptoms:
Differential diagnosis includes Heartwater, Contagious Caprine Pleuropneumonia, and Nairobi Sheep Disease.
Treatment and Control
There is no specific treatment, which must therefore be symptomatic.
The veterinary authorities must be notified at once of any symptoms in goats and sheep suggestive of PPR, as the disease is not endemic in Kenya . Immediate control by restriction of movement of susceptible animals and vaccination is essential, using an attenuated PPR vaccine. Sick animals should be immediately isolated and contact animals vaccinated. In the event of an outbreak regulation of markets and movement is vital in the mechanics of control.
The veterinary authorities must be notified at once of any symptoms in goats and sheep suggestive of PPR, as the disease is not endemic in Kenya . Immediate control by restriction of movement of susceptible animals and vaccination is essential, using an attenuated PPR vaccine. Sick animals should be immediately isolated and contact animals vaccinated. In the event of an outbreak regulation of markets and movement is vital in the mechanics of control.
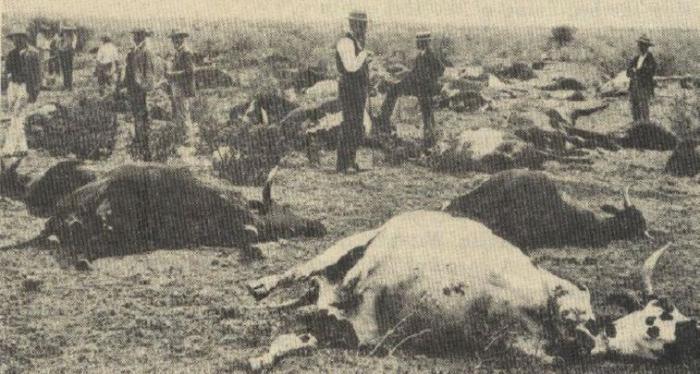 |
| Rinderpest in the past - now eradicated. |
| © Dr. Hugh Cran, Nakuru, Kenya |
Introduction
Rinderpest has recently been eradicated from the world. However it is important for farmers to be aware of this devastating disease, along with others of a similar nature such as Peste des Petits Ruminants which is caused by a virus closely related to the one that causes Rinderpest.
Rinderpest is a disease of cloven-hoofed animals, characterized by fever, erosions in the mouth, irritation, pain and swelling of the mucous membrane of the stomach and intestines, a foul odour, dehydration and death. In epidemic form it is/was the most deadly plague known in cattle. When the disease entered north-east Africa at the end of the 19th century it devastated the cattle and ruminant wildlife from Somalia to South Africa, killing millions of animals as it spread.
All cloven-hoofed animals are probably susceptible, but cattle, buffalo, giraffe, wild pigs and various species of antelope are/were most often affected.
The virus is closely related to that of Measles, Canine Distemper and Peste des Petits Ruminants of sheep and goats.
Mode of spread
Transmission is by contact, the virus being passed from sick to healthy animals in the air they breathe out, in nasal and oral discharges and in the faeces. Infected droplets are inhaled and the virus penetrates through the mucosa of the upper respiratory tract. There is no carrier state and the virus maintains itself by continual transmission among at-risk animals.
Signs of Rinderpest
- An incubation period of 3-15 days is followed by a fever, loss of appetite, depression, and a discharge from the eyes and nose.
- Within 2-3 days, pinpoint decaying wounds appear on the gums. These soon enlarge to become cheesy plaques affecting the gums, inside of the lips and tongue, and often also the roof of the mouth.
- The discharges from the nose and eyes have mucous and pus and smell foul, and the muzzle appears dry and cracked.
- The final clinical sign is profuse diarrhoea with an offensive smell, often containing mucous, blood and shreds of mucous membranes. There are signs of abdominal pain, sunken eyes, straining, dehydration, general weakness, collapse and death.
- In epidemic areas the number of animals affected was often 100% and the death rate up to 90%.
- Post-mortem signs of decay and erosion are seen throughout the gastro-intestinal and upper respiratory tract with classic "zebra-striping" in the rectum.
Diseases with similar symptoms
The two diseases with which Rinderpest might be confused are the fatal Mucosal Disease syndrome of Bovine Viral Diarrhoea (see above) of cattle and Peste des Petits Ruminants (see above) in goats and sheep.
Prevention - Control - Treatment
Thanks to the development of highly effective vaccines, large scale vaccination campaigns and national and continental control and eradication strategies this devastating animal disease has vanished into the history books. Its elimination should serve as a shining example of what can be done when veterinary science and international political will join forces.
2. Review by Hugh Cran March 2010 - Jan 2011
3. Review workshop team. Nov 2 - 5, 2010
4. Addition of Pest of small Ruminants By Dr Hugh Cran Oct 2011
- For Infonet: Anne, Dr Hugh Cran
- For KARI: Dr Mario Younan KARI/KASAL, William Ayako - Animal scientist, KARI Naivasha
- For DVS: Dr Josphat Muema - Dvo Isiolo, Dr Charity Nguyo - Kabete Extension Division, Mr Patrick Muthui - Senior Livestock Health Assistant Isiolo, Ms Emmah Njeri Njoroge - Senior Livestock Health Assistant Machakos
- Pastoralists: Dr Ezra Saitoti Kotonto - Private practitioner, Abdi Gollo H.O.D. Segera Ranch
- Farmers: Benson Chege Kuria and Francis Maina Gilgil and John Mutisya Machakos
- Language and format: Carol Gachiengo
- Barber, J., Wood, D.J. (1976) Livestock management for East Africa: Edwar Arnold (Publishers) Ltd 25 Hill Street London WIX 8LL
- Blood, D.C., Radostits, O.M. and Henderson, J.A. (1983) Veterinary Medicine - A textbook of the Diseases of Cattle, Sheep, Goats and Horses. Sixth Edition - Bailliere Tindall London. ISBN: 0702012866
- Blowey, R.W. (1986). A Veterinary book for dairy farmers: Farming press limited Wharfedale road, Ipswich, Suffolk IPI 4LG
- FAO Rome 1968: Emerging Diseases of Animals. The Enterotoxaemias of Sheep caused by organisms of the Welch Group
- Force, B. (1999). Where there is no Vet. CTA, Wageningen, The Netherlands. ISBN 978-0333-58899-4.
- Hall, H.T.B. (1985). Diseases and parasites of Livestock in the tropics. Second Edition. Longman Group UK. ISBN 0582775140
- Hunter, A. (1996). Animal health: General principles. Volume 1 (Tropical Agriculturalist) - Macmillan Education Press. ISBN: 0333612027
- Hunter, A. (1996). Animal health: Specific Diseases. Volume 2 (Tropical Agriculturalist) - Macmillan Education Press. ISBN:0-333-57360-9
- ITDG and IIRR (1996). Ethnoveterinary medicine in Kenya: A field manual of traditional animal health care practices. Intermediate Technology Development Group and International Institute of Rural Reconstruction, Nairobi, Kenya. ISBN 9966-9606-2-7.
- Khan CM and Line S (2005): The Merck Veterinary Manual, 9th Edition, Merck & Co Inc Whitehouse Station NJ USA
- Martin WB (Editor)1983: Diseases of Sheep. Blackwell Scientific Publications ISBN 0-632 -01008 -8
- Mugera, Bwangamoi & Wandera 1979: Diseases of Cattle in Tropical Africa. Kenya Literature Bureau Nairobi
- Onderstepoort Henning 1956: Animal Diseases in South Africa 3rd Edition
- Pagot, J. (1992). Animal Production in the Tropics and Subtropics. MacMillan Education Limited London
- Poisoning in Veterinary Practice Prof. E GC Clarke The Association of the British Pharmaceutical Industry 106 Regent Street London WIR 6DD 1975
- Sewell MMH and Brocklesby DW (editors)(1990): Handbook on Animal Diseases in the Tropics, 4th Edition 1990. Balliere and Tindall, 24-28 Oval Road, London NW1 7DX, UK. ISBN NO: 0-7020-1502-4
- Sewell and Brocklesby, Editors 1990: Handbook on Animal Diseases in the Tropics 4th Edition. Bailliere Tindall ISBN 0-7020-1502-4
- The African Veterinary Handbook Mackenzie & Simpson 1964 Pitman, Nairobi
- The Merck Veterinary Manual 9th Edition Kahn & Line 2005 ISBN 0-911910-50-6
- The Organic Farmer magazine No. 50 July 2009
- The Organic Farmer magazine No. 51 August 2009
- Veterinary Medicine A Textbook of the Diseases of Cattle, Sheep, Pigs, Goats and Horses 1983 6th Edition Blood, Radostits and Henderson ELSB & Bailliere Tindall ISBN 0-7020-0988-1